18,600
18,6
1,390
1,39
630
63
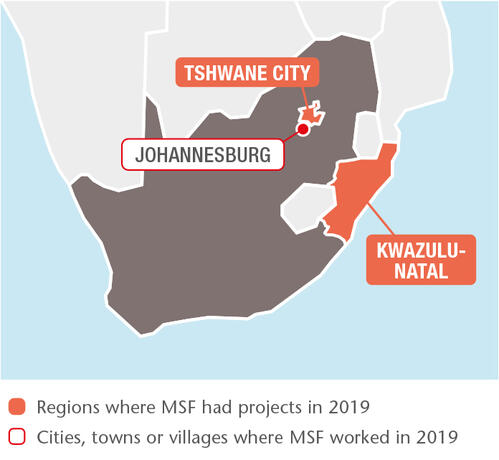
In 2019, our large-scale community HIV/TB project in King Cetshwayo district, KwaZulu-Natal, run in collaboration with the Department of Health, became the first in South Africa to reach the UNAIDS 90-90-90 targets.The globally agreed 90-90-90 targets require that 90 per cent of people living with HIV know their status; that 90 per cent of people diagnosed with HIV initiate and remain on ARV treatment; and that 90 per cent of people on ARV treatment reach and maintain an undetectable viral load by 2020. A survey supported by Epicentre, MSF’s epidemiological research arm, revealed that 90 per cent of people living with HIV knew their status, 94 per cent of those were on antiretroviral treatment, and 95 per cent of people on treatment had a suppressed viral load. In response to the growing phenomenon of disengagement from HIV care, we have developed services in the urban slum of Khayelitsha to encourage patients, including those with advanced HIV, to restart treatment. In Khayelitsha and rural Eshowe, where young people, particularly women, remain highly vulnerable to HIV, we offered preventive treatment to 204 patients. We also continued to develop different HIV screening strategies, including distributing over 30,000 oral self-testing kits.
MSF supports two multinational, multi-site clinical trials: TB PRACTECAL and endTB, which aim to find shorter, less toxic and more effective treatment regimens for multidrug-resistant TB. In 2019, the endTB trial enrolled its 48th patient at the Khayelitsha site, and two new sites, Durban and Johannesburg, were added to the TB PRACTECAL trial, with a total of 70 patients enrolled by the end of the year. We welcomed the registration of the newer TB drug delamanid, and we continue to push for improved treatment for the disease nationally.
Sexual violence
MSF works with the provincial health department to provide victims of sexual violence with essential medical and psychosocial care through community clinics known as Kgomotso Care Centres on South Africa’s platinum mining belt. In 2019, we handed over two of the four clinics to the department. We also launched initiatives to identify victims of sexual violence, for example through our school health programme, which reached 26,000 students. Community-based initiatives accounted for at least 160 of the 1,294 new patients seen in 2019.
To meet the high demand for pregnancy termination, we trained 23 health department providers in safe abortion care. In MSF-supported facilities, an average of 209 abortions were performed monthly in 2019.
Migration
In Tshwane, we opened a hub offering medical and psychosocial care to migrants, refugees and asylum seekers, who struggle to access public health services under South Africa’s increasingly restrictive migration policies. In 2019, 668 people received medical and psychological support and 456 attended group mental health sessions. In addition, our emergency teams responded to episodes of xenophobic violence against migrants in three provinces.
Access to medicines
We continue to call for wider availability of lifesaving drugs by addressing the patent, registration and financial barriers that prevent their supply. Through a national access programme set up by MSF, we donated 610 courses of flucytosine – an effective cryptococcal meningitis treatment not yet registered for use in South Africa – to 15 specialist facilities across the country. The programme seeks to build evidence to support its registration as an essential medicine.
227
227
€11.9 M
11.9M
1986
1986
¹The globally agreed 90-90-90 targets require that 90 per cent of people diagnosed with HIV know their status; that 90 per cent of people living with HIV initiate and remain on ARV treatment, and that 90 per cent of people on ARV treatment reach and maintain an undetectable viral load by 2020.