23,700
23,7
4,120
4,12
1,100
1,1
HIV prevalence in Malawi is over 10 per cent among people aged 15 to 64, one of the highest in the world. The country’s HIV programme has achieved significant success, with over 80 per cent of the one million people who have tested positive being started on treatment. However, more robust strategies are required to prevent infection and reduce mortality among more at-risk patients.
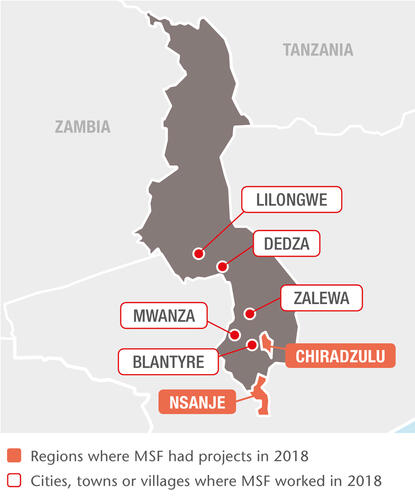
HIV care in Chiradzulu and Nsanje
In rural Chiradzulu district, we focus our HIV activities on complex cases such as patients on second- or third-line antiretroviral (ARV) therapy and those with opportunistic infections or facing treatment failure. In 2018, our teams provided care to almost 5,500 patients, of whom 2,500 were children and adolescents.
Our services include decentralised outpatient clinics, ‘teen clubs’ for adolescents, point-of-care tests, counselling and inpatient care.
In Nsanje, where we have teams in 10 health facilities, we are supporting the health ministry to increase early access to treatment and decentralised models of care involving the community.
Around 25 to 30 per cent of HIV patients seek medical care only when they are already in advanced stages of the disease, increasing the risk of opportunistic infections or even death. The majority are already on ARV treatment yet struggle with daily treatment or have developed resistance to their medication.
Cervical cancer
Cervical cancer accounts for 40 per cent of all cancers among women in Malawi and kills an estimated 2,314 a year. We are developing a comprehensive cervical cancer programme, comprising screening, diagnosis, vaccination, treatment, surgery, chemotherapy, radiotherapy and palliative care.
In 2018, we screened more than 11,000 women in Blantyre and Chiradzulu districts and started building a cervical cancer clinic in Queen Elizabeth hospital, the main university teaching hospital in Malawi. It will open in 2019, with an operating theatre, an 18-bed inpatient ward and a day clinic; services such as vaccinations, chemotherapy and radiotherapy will be added progressively.
Healthcare for prisoners and sex workers
We handed over our HIV, tuberculosis (TB) and primary healthcare services in Maula, Chichiri, Dedza and Kachere prisons to the prison authorities and partner organisations, with an ‘operational toolkit’ documenting the key components of healthcare provision in a prison setting, so that the model can be implemented elsewhere. Over 400 inmates benefited from our HIV and TB services in 2018.
Since 2014, we have also been working to increase access to HIV, TB and sexual and reproductive healthcare services for women engaged in sex work around trade centres and along transport routes in Dedza, Mwanza, Zalewa and Nsanje districts.
Our project data has shown that female sex workers are almost six times more likely to contract HIV than other women but face greater challenges in accessing health services. By the end of 2018, 4,784 sex workers had been enrolled in the project, including 850 women living with HIV, of whom 80 per cent are receiving ARV treatment.