197,600
197,6
38,500
38,5
11,100
11,1

3,780
3,78
Although the conflict subsided in late 2017 and increasing numbers of displaced people returned to their areas of origin in 2018, significant barriers to returning remain.<a href="http://iraqdtm.iom.int/">IOM Iraq Displacement Tracking Matrix</a> Many displaced families lack the necessary documentation, properties and livelihoods have been damaged if not destroyed, and security concerns persist in some areas. The context remains complex and unpredictable, due to ongoing political disputes, tribal conflicts and attacks by armed groups.
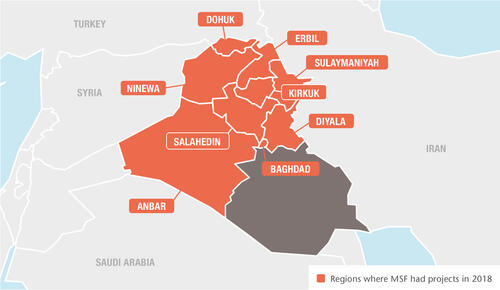
In 2018 in Iraq, Médecins Sans Frontières (MSF) continued to offer services ranging from basic healthcare and treatment for non-communicable diseases (NCDs), to maternity, paediatric and emergency care, surgery and mental health support, for displaced people, returnees and communities most affected by violence. We also rehabilitated and equipped hospitals and clinics in some of the most war-affected regions to help get the Iraqi health system back on its feet.
Anbar governorate
We continued to provide primary healthcare, treatment for NCDs and mental health services, including psychiatric care, in two camps for internally displaced people (IDPs), handing over activities in the second half of the year as the camp populations gradually decreased and other organisations started providing medical services.
In April, we opened an outpatient clinic at Ramadi teaching hospital to treat patients with moderate and severe mental health disorders.
Baghdad governorate
Our teams in Baghdad Medical Rehabilitation Centre provided post-operative rehabilitation to 261 severely injured patients in 2018, including physiotherapy, pain management and mental healthcare.
We also completed the rehabilitation of Imam Ali hospital’s emergency department, in Sadr city, with the installation of high-quality medical equipment and a new triage system, supplied 60,000 tablets of first-line medication to Iraq’s national tuberculosis (TB) programme, and donated a GeneXpert machine to Rusafa chest and respiratory clinic to improve the detection of drug-resistant TB.
Diyala governorate
MSF teams offered treatment for NCDs, mental health support and sexual and reproductive healthcare in Jalawla and Sadiya primary health centres for families returning to the area, and in camps for displaced people in Khanaqin. We also ran health education sessions on chronic and endemic diseases, sexual and reproductive health, and psychological first aid.
Erbil governorate
We provide psychological, psychiatric and psychosocial care in four different camps around Erbil, and to displaced people and host communities in Kalak. We reduced our activities in October as the camp populations declined, concentrating on moderate to severe mental health cases and treatment for NCDs.
Kirkuk governorate
As displaced people continued returning to Hawija, one of the areas most affected by conflict, our teams conducted some 14,500 outpatient consultations, as well as treatment for NCDs and health education sessions in Al-Abassi and Hawija city. We also provided mental healthcare in Al-Abassi, and rehabilitated the water stations in Al-Shazera and Al-Abassi to ensure clean drinking water and to prevent outbreaks of water-borne diseases.
We continued to run basic medical and mental healthcare in Daquq camp until it closed in September, and offered technical support and training at Hawija hospital in the emergency room, laboratory and maternity department and in infection prevention and control.

Ninewa governorate
Several neighbourhoods in Mosul still lie under piles of rubble, and thousands of people struggle to access basic services such as healthcare, water and electricity. In 2018, we scaled up our medical activities in both east and west Mosul in response.
In Nablus, west Mosul, we ran a comprehensive maternity unit with surgical capacity for caesarean sections, paediatric healthcare (including for newborns), stabilisation and referrals for emergencies and mental health services. Our teams assisted more than 5,300 normal deliveries, performed 1,120 caesarean sections and treated 34,500 patients in the emergency room.
In April, we opened a comprehensive post-operative care facility in east Mosul for patients with violent or accidental trauma injuries. The facility has a mobile operating theatre, a 20-bed inpatient ward, 11 recovery rooms, a mental health department and a rehabilitation unit.
In July, we launched a programme specifically aimed at increasing access to mental healthcare and psychosocial aid. Working in three health centres, our teams provide counselling, psychosocial first aid, psychosocial support and referrals for psychiatric care.
At the end of the year, we also completed the rehabilitation of Al-Salam hospital’s 24-hour emergency department, which now has two wards, a trauma room, a pharmacy, two consultation rooms and a triage area.
South of Mosul, we provide emergency consultations, intensive care, treatment for burns and mental healthcare for the resident and displaced population of Qayyarah sub-district and the surrounding area.
Our 62-bed hospital has an inpatient department, a paediatric ward and an inpatient therapeutic feeding centre. As the healthcare needs of displaced people and those returning to the area continued to grow in 2018, we expanded our burns and neonatal activities and set up a second operating theatre. Our teams performed more than 18,000 emergency room consultations and almost 2,500 surgical interventions during the year.
We also started providing primary healthcare in Qayyarah Airstrip camp at the beginning of 2018, including outpatient treatment for malnutrition, mental healthcare, sexual and reproductive health services, and referrals. In July, we added a 24-hour emergency room.
In August, we completed the rehabilitation of Sinuni hospital, in Sinjar district, where medical activities were significantly limited during the conflict. It reopened with a fully equipped emergency room, maternity unit, inpatient paediatric ward and mental health services.
We also continued to provide emergency maternity and neonatal care, basic paediatrics, emergency stabilisation services and mental health support in Tal Maraq health facility, Zummar sub-district.
Salahedin governorate
For the first six months of the year, we conducted outpatient and mental health consultations for returnees and displaced people through our mobile clinics in Tikrit and managed a primary healthcare centre in Al-Allam camp. Following a reduction in the number of displaced people and an increase in activities by other organisations, we handed over these activities to the Iraqi Department of Health in June.
Emergency response activities
After several cases of Crimean-Congo haemorrhagic fever were reported in different regions of Iraq, we rapidly deployed a team of experts to support hospitals. In July, 228 Iraqi doctors, nurses and cleaners were trained in five public hospitals in Diwaniyah, Najaf, Babel and Baghdad governorates.
We also supported the Department of Health to vaccinate more than 111,000 children aged six months to 15 years old in response to a measles outbreak in Ninewa governorate in July.
Rasmiyya’s story
In 2004, following the US invasion, Rasmiyya lost four of her sons in the bombing of their home city of Fallujah. Another of her sons has been jailed since 2006, accused of collaborating with militants.
“I fled Fallujah with my son Mohammad, on 8 January 2014. We went to Baghdad.” For a time, her husband refused to leave Fallujah in spite of the bombing, but in 2015 she convinced him. “I didn’t recognise him, he was so thin. And after two months in Baghdad, he died. We had no money, and there were no adequate medical services for us.”
In October 2016, Rasmiyya had little choice but to move to Amriyat Al-Fallujah camp for internally displaced people. “My son Mohammad, who came with me to the camp, was lucky to find a job in a factory nearby. But three months ago, a group of armed men arrived in a car and took him away. I’ve had no news of him since.”
Rasmiyya’s four daughters and one other son live in Baghdad. “I wish I could fly there to see them. The checkpoints surrounding the camp prevent me from leaving.”