1,826,300
1,826,3
776,600
776,6
102,600
102,6

38,200
38,2
34,300
34,3
9,100
9,1

7,760
7,76
6,950
6,95
6,910
6,91
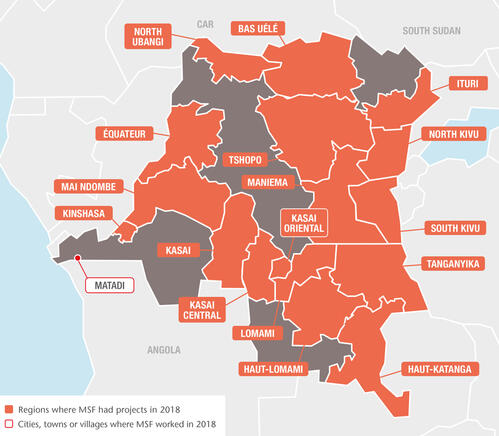
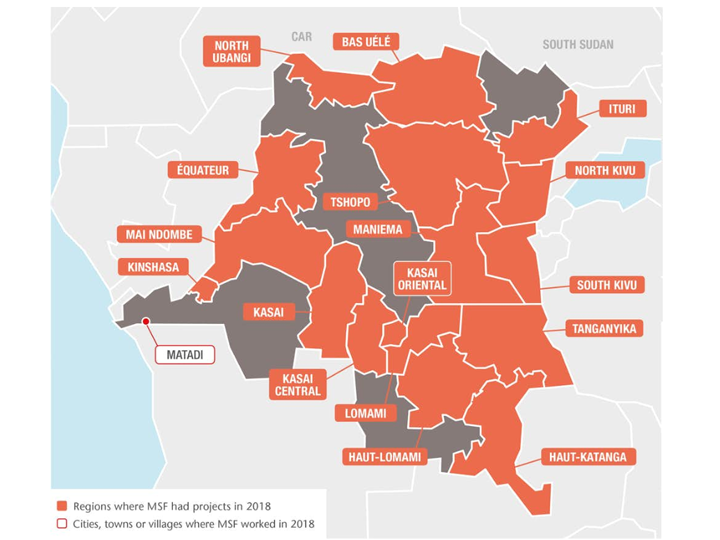
Médecins Sans Frontières (MSF) ran 54 medical projects in 17 of the Democratic Republic of Congo’s 26 provinces in 2018. With services ranging from basic healthcare to nutrition, paediatrics, treatment for victims of sexual violence and care for people living with HIV/AIDS, we provide comprehensive medical assistance where it is needed most. We responded to nine measles outbreaks and two successive outbreaks of Ebola in 2018, including the country’s largest ever, which was still ongoing at the end of the year.
Assisting displaced and host communities
Since 2016, approximately 1.4 million people have been displaced by violence in Greater Kasai region. In 2018, our teams in the region supported referral hospitals in Kakenge, Kananga, Tshikapa and Tshikula, as well as 35 health centres in the surrounding areas, with nutritional, paediatric and maternal healthcare, surgery for violent trauma, treatment for victims of sexual violence, and referrals. In Kamonia health zone, southern Kasai province, we also provided medical assistance to Congolese people forced out of neighbouring Angola.
We conducted more than 80,000 medical consultations in Bunia city and in Djugu territory, Ituri province, where intercommunal clashes and fighting between armed groups caused further largescale displacement. We also built latrines and showers, responded to outbreaks of measles and cholera, and treated victims of sexual violence.
We continued to assist people displaced by violence in 2017 in Kalémie, Tanganyika province, providing relief items and water together with community-based healthcare and psychological support. We also set up new primary and secondary healthcare services for victims of violence and displacement in Salamabila, Maniema province, and Kalongwe, in South Kivu.
At the end of the year, we sent an emergency team to assist many thousands of people fleeing extreme violence in the region around Yumbi, in Mai-Ndombe province in the west of the country.
To assist refugees from the Central African Republic who had crossed into northern DRC, we supported hospitals and health centres in Gbadolite and Mobayi-Mbongo, North Ubangi province, and ran mobile clinics that also served the local community. In Bili, in the same province, we supported emergency, paediatric and neonatal services in the referral hospital and in 50 health centres and health posts with an integrated community approach.
Over to the east, along the border with South Sudan, we treated more than 48,000 refugees in the informal sites of Karagba and Ulendere.

Comprehensive care in the Kivu provinces
In the Kivu provinces, in eastern DRC, which have been plagued by conflict for over 25 years, we maintain a number of long-term projects that ensure continuity of care while also launching emergency responses to violence-related trauma and displacement.
In North Kivu, our teams run comprehensive medical programmes in Lubero, Masisi, Mweso, Rutshuru and Walikale, supporting the main reference hospitals and peripheral health centres to deliver both basic and secondary care. Services include emergency and intensive care, surgery, nutrition and maternal and paediatric healthcare, community-based healthcare, and outreach activities such as mass vaccination in hard-to-reach areas.
In South Kivu, we offer treatment for malaria, HIV, tuberculosis, malnutrition, acute respiratory infections and diarrhoeal diseases to refugees, displaced people and local communities. We had teams working in more than a dozen facilities across the province, including a new health centre in Kusisa. Constructed in 2018, it offers maternity, paediatric and emergency wards and an operating theatre.

Treating victims of sexual violence
In Kananga, in Kasai Central province, we treated between 200 and 250 victims of sexual violence each month in 2018, mostly women but also men and young children.
We also set up psychological and medical services for victims of sexual violence in a hospital and four health centres in Salamabila, in Maniema province, and increased services in another six health centres around Mambasa, in Ituri province, piloting mobile apps to help improve the provision of treatment for 5,500 patients suffering from sexually transmitted infections and victims of sexual violence.
We also run a clinic for victims of sexual violence in Walikale, North Kivu, where we provide medical and mental healthcare and family planning services.

Responding to epidemics
Responding to epidemics is a core activity for MSF in DRC, and in 2018 our emergency teams conducted surveillance and initial diagnosis from 10 sites across the country, resulting in multiple emergency interventions.
We responded to nine measles outbreaks affecting Haut-Uélé, Ituri, former Katanga, Kasai, Maniema, and Tshopo provinces throughout the year, providing care and supporting the Ministry of Health to contain the spread.
We also supported the ministry’s response to large cholera outbreaks affecting many areas, including cities such as Kinshasa, Lubumbashi, Ngandajika and Mbuji-Mayi.
In Maniema, we continue to support the Ministry of Health with the management, active case finding and treatment of sleeping sickness (human African trypanosomiasis).
HIV/AIDS remains another deadly threat in the country, with alarming numbers of people presenting in such an advanced stage of the disease that they need immediate hospital care or are too late for treatment.
We run a major HIV/AIDS programme at the Centre Hospitalier de Kabinda in Kinshasa, where we provided care for more than 2,000 people in 2018, including patients with advanced HIV. Our teams support the HIV/AIDS activities of two other hospitals in Kinshasa, and run HIV-mentoring programmes in three of the city’s health centres. We also provide technical and financial support to five health facilities in Goma, including Virunga general hospital, to improve the provision of HIV care and increase access to antiretroviral treatment.
Ebola response activities
The epidemic has proven extremely hard to control, despite a massive mobilisation of resources. Serious doubts have been cast over the approach taken and its failure to meet people’s expectations and needs. The infection rate has been steadily picking up and the responders have struggled to earn the population’s trust, prompting a re-thinking of the response strategy as we entered 2019.

2,800
2,8
450
45
The first Ebola outbreak was declared on 8 May in Équateur province, in northwestern DRC. Médecins Sans Frontières (MSF) supported the Congolese Ministry of Health in Bikoro, Itipo, Mbandaka and Iboko, providing care to 38 confirmed patients, 24 of whom survived and returned to their homes. Sadly, 14 died. More than 120 other patients showing symptoms consistent with Ebola were isolated and tested but found not to have the virus.
Teams from MSF, the World Health Organization (WHO) and the Congolese Ministry of Health vaccinated a total of 3,199 people using an investigational vaccine approved by the WHO under the framework for expanded access/compassionate use.
Around Bikoro and Itipo, our teams alone vaccinated 1,673 people considered to be most at risk of contracting the virus, including first- and second-line contacts of confirmed Ebola patients and frontline workers (health workers, burial workers, traditional healers and motorbike taxi drivers).
On 24 July, the Ministry of Health declared the end of the outbreak. The following week, on 1 August, a second one was declared, this time in the northeastern province of North Kivu.Laboratory tests found that both outbreaks were caused by the Zaire species of the virus, but by two different strains of it – meaning the outbreaks were unrelated.
We participated in the response immediately, investigating the first alert and setting up an Ebola treatment centre in Mangina, the small town where the outbreak was declared. We then opened a second treatment centre in Butembo, a city of one million people which became a hotspot later in the year.
We progressively increased the level of care provided, and from the early stages of the outbreak were able to offer the first-ever potential therapeutic treatments, under an emergency WHO protocol.

As in Équateur, we contributed to the intervention by vaccinating frontline workers, while the WHO and Ministry of Health vaccinated first- and second-line contacts. We also helped local health centres to prevent and control infections, by setting up triage zones and decontaminating facilities where a positive case had been reported. An MSF rapid response team was sent to investigate alerts.
By the end of the year, over 600 confirmed and suspected cases had been reported and more than 360 people had died. The outbreak was not yet under control and the struggle continued in the face of numerous challenges. With new cases appearing in scattered clusters, the epicentre has moved multiple times.
The high mobility of people in the region, and the fact that some new cases are not linked to any previously known chains of transmission make it even harder to trace contacts and control the evolution of the outbreak. As does the fact that this is all happening in a conflict zone: insecurity prevents full access to certain areas and episodes of violence have interrupted activities, potentially causing precious ground to be lost.
Our missing colleagues
On 11 July 2013, four MSF staff were abducted in Kamango, in the east of DRC, where they were carrying out a health assessment. One of them, Chantal, managed to escape in August 2014, but we are still without news of Philippe, Richard and Romy. We remain committed to obtaining their release.