The conflict in Borno State started in 2009 when Boko Haram (BH) launched attacks in northeastern Nigeria. By 2014, BH controlled large swathes of territory in Borno State and caused large-scale population displacement. In 2015, Nigeria elected a new President who vowed to take back control of all Nigerian territory from BH. Since then, the Nigerian army escalated their operations and have been engaged in active fighting with BH across Borno, including launching airstrikes in areas under BH control. This has caused further mass displacement of the population, particularly towards Maiduguri, the capital of Borno State. Already a large city, the population of Maiduguri has doubled with the arrival of internally displaced people (IDPs), with over 2 million people now living in the city and its immediate surroundings.
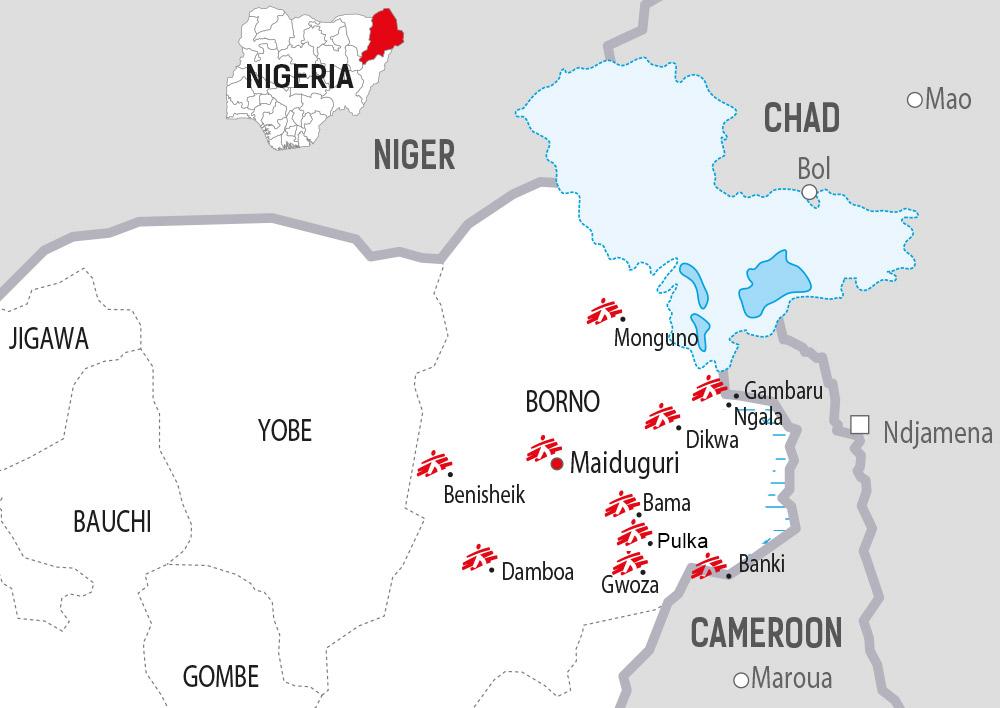
The military has taken back some cities and towns outside Maiduguri and is controlling them, meaning that the people within them live under military control, sometimes with little or no possibility to move outside. The government has reiterated its intention to bring all the countryside of Borno under military control in the imminent future, so fighting may continue to impact large areas of the state, affecting an unknown number of people living within those areas. In border areas, the Nigerian army receives military assistance from neighbouring countries Chad, Cameroon and Niger.
As a result of the conflict, 2.6 million people are displaced and 480,000 children are suffering from severe acute malnutrition across the four countries (Nigeria, Cameroon, Chad and Niger) according to OCHA.
A total of 1.8 million people are currently displaced in northeastern Nigeria, including an estimated 1.1 million in Maiduguri alone; 4.4 million people are food insecure according to OCHA.
In Borno State, more than 40 per cent of the health facilities are known to be destroyed, many of them found to have been burned during the armed conflict (Borno State Ministry of Health) http://www.who.int/health-cluster/news-and-events/news/Borno-Health-Sector-Bulletin-Issue3.pdf?ua=1.

Maiduguri
Today, more than 1.1 million IDPs are living in Maiduguri (according to the International Organization for Migration), 90 per cent of them within the host community while the other 10 per cent are accommodated in more than 10 official camps and multiple informal camps and settlements.
MSF focuses on maternal and child health in Maiduguri, running an inpatient therapeutic feeding centre (ITFC) in Gwange district and two large health centres in the districts of Maimusari and Bolori. The Maimusari health centre also includes a pediatric emergency room and inpatient facility. A mobile team runs food distributions and offers medical and nutritional care and vaccination in four informal camps.
Gwange ITFC and ATFC
In Gwange, we have an ITFC with a 110-bed capacity in the compound of the Ministry of Health-run health centre. The ITFC is under five tents, each constituting one ward: admission/triage, an intensive care unit, an isolation ward for children with infectious diseases, an acute phase ward, and a transition/rehabilitation ward. The centre only admits severely malnourished children with complications. Around 300 children are admitted per month, including children over the age of five. To compensate for the lack of food, we started in late September to give a family food ration to each family with a child released from the ITFC. The plan is to increase to 150 beds and to routinely admit children over the age of five. An ambulatory therapeutic feeding centre (ATFC) was opened early November to help with the continuity of care.
Maimusari and Bolori health centres
In Maiduguri, we run two heath centres, Maimusari and Bolori. In these centres we run paediatric outpatient departments (OPDs), ATFCs, and maternity units that provide antenatal and postnatal consultation and assist normal deliveries. In Maimusari, there is also a pediatric inpatient department (26 beds), a pediatric intensive care unit (15 beds) and an emergency room.
Patient numbers increased substantially in September and October, with over 1,000 patients per day being consulted in the OPDs, and on some days more than 700 patients in Maimusari alone (nearly 6,000 consultations per week in both facilities combined). About half of the patients are children under the age of five. People come from all over the city and are already lining up at 6am, even though the health centres do not open until 8am. Lack of free healthcare in Maiduguri is one important reason for this; people have to pay in the state health system and often report being sent away when they don´t have the financial means.
Almost half of the patients under five years of age consulted in Maimusari are malnourished. In the week from 10 to 16 October, more than nine per cent of the patients suffered from severe acute malnutrition (SAM) and an additional 31 per cent from moderate acute malnutrition (MAM). About 1,000 children are followed in the outpatient malnutrition programmed (ATFC), with 200 to 300 new admissions each week. Currently, only children under 5 years of age are screened and treated for SAM, but this will be expanded to older children and those with moderate levels of malnutrition. The team is also preparing to start a distribution of food rations for families with children in the ambulatory feeding programmed in Maimusari (currently 800 children enrolled).
The number of deliveries and antenatal care consultations has also been increasing. In both facilities together, pregnant women receive more than 1,000 antenatal care consultations per week. In Maimusari, about 120 women deliver their babies per week.

The camps
There are still some IDPs arriving in Maiduguri, especially to Muna Garage camp. The relocation of IDPs from Maiduguri to their towns of origin with the army’s assistance has slowed down since the fighting re-escalated at the end of October and most came back to Maiduguri because they did not find adequate living conditions outside. Yet the Nigerian government has repeatedly announced that it intends to close down all IDP camps by the end of May 2017. At the end of September, several camps in school buildings have been closed, as schools reopened after more than two years’ closure due to BH attacks against schools. The IDPs were moved to other camps inside or outside Maiduguri. In Maiduguri, MSF is conducting a health surveillance activity now covering all official camps and the two largest unofficial camps of Muna Garage and Custom House, where mortality rates, especially for children under five, remain a concern.
MSF teams are currently supporting IDPs in four informal camps: Muna Garage (around 14,500 IDPs sheltering in makeshift self-built shelters set up on private land) and Custom House (around 8,000 IDPs sheltering in unfinished buildings and makeshift shelters), both located at the eastern outskirts of Maiduguri at the road towards Dikwa, as well as Nursing Village in Maisandari district (around 2,000 IDPs) and Fariya (around 3,600 IDPs).
The mobile food distribution team started in Muna Garage and Customs House camps in September and were extended in October to smaller camps. MSF regularly distributes millet, beans and palm oil to the inhabitants of the camps, as well as ready-to-use therapeutic food for families with malnourished children. Teams arrange for referral of children requiring inpatient care to our MSF facilities, offer outpatient medical treatment, provide seasonal malaria chemoprophylaxis, and aim to vaccinate all children under five against measles and pneumococcal disease. MSF has also distributed aid kits (mosquito nets, jerry cans, soap, mats, and blankets).
At the beginning of September, MSF teams had recorded a rate of severe acute malnutrition among children under five above five per cent in Customs House camp. Following the food distributions, malnutrition mass screening showed a decreasing trend in severe malnutrition.
Monguno
In Monguno, the current estimated population is 225,000 people. An estimated 68,000 IDPs have been living in nine camps in Monguno, according to the State Emergency Management Agency (SEMA), with another 60,000 IDPs living among the host community. During October, new arrivals continued. There had been almost no healthcare provision for over a year in the town. Now, there are five medical organisations present, including MSF. Given the lack of secondary healthcare, MSF has set up an ITFC (around 12 admissions per week), a paediatric IPD (around 40 admissions per week) and an emergency room under tents with an overall capacity of 50 beds. Patient numbers have increased, yet the facility is not full at the moment, partly as the admission criteria were set initially for children under five and partly because of the lack of training of local health workers to recognise and refer acute paediatric illness. In September, 389 patients were treated in the emergency room, 70 per cent of them children under five. The main illnesses treated are malaria, respiratory tract infections and measles. The teams will start an OPD at the end of October.
Bama
Bama, once the second-most populated town in Borno State, is now held by the army. An IDP camp is located inside the compound of the hospital, and is under military control. Around 8,000 people are currently living in the camp, mostly women and children under the age of five. They live in makeshift shelters made out of iron sheeting taken from surrounding destroyed houses and are totally dependent on outside assistance, including for food. No one lives outside the camp; the town is otherwise empty. The catastrophic situation of the IDPs in the camp has improved with regular food distributions, including from MSF, and the provision of healthcare and nutritional services in the camp. The once extremely high malnutrition rates are now below the emergency threshold. The Governor of Borno temporarily relocated his office to Bama for several days at the end of September in a symbolic move, but the rehabilitation of houses (which were all burnt) has not yet begun.

The latest intervention of the mobile MSF team in Bama happened from 19 to 22 October. They distributed millet, beans, oil and soap to 1,800 families with children under five. A screening of 2,058 children for malnutrition now demonstrates 2.0 per cent SAM and 7.7 per cent MAM. This is about the same rate recorded in September, with the 22 new SAM cases, mainly new arrivals. The team treated the malnourished children, gave seasonal malaria prophylaxis to more than 1,000 children, and provided a second round of pneumococcal vaccination. They also dug six soak-away pits for the six boreholes and constructed two solar boreholes and water towers.
When an MSF team originally visited Bama with a military escort on 21 June, they found a population in a catastrophic situation: out of the 800 children screened, 19 per cent were suffering from SAM. Counting of the graves in the cemetery behind the camp showed more than 1,200 graves dug since the IDPs had been gathered in the hospital compound. The team returned in July, August, September and October to distribute food and provide medical and nutritional care. During the rainy season, there have been few new arrivals to the camp, and some of the population was moved to other camps (including to Banki). Bama provides a good example of the possibility of rapid stabilisation of a situation if adequate food and medical aid is provided; however, the situation could again rapidly deteriorate if access is lost due to insecurity.
Dikwa
Dikwa is an enclave controlled by the military. Most of the town is destroyed. The population is now estimated at around 70,000 IDPs, but could be higher. Around 21,000 IDPs are living in the community; 49,000 are living in about 14 camps, but only three of the camps are well-defined and organised. There is an UNICEF-supported clinic in the town and health posts in two camps. The people are almost completely dependent on ICRC food rations distributed by the Nigerian Red Cross. The town had been mainly deserted in 2014 and 2015, with only around 12,000 people remaining in a camp. Water is a big concern, both in quantity and quality. Rates of severe acute malnutrition in a recent screening done by UNICEF were very high (14 per cent).
An MSF team visited the town in mid-July (under armed escort) and at the beginning of October (by helicopter). Based on the findings, the team returned to Dikwa on 26 October for four days for a nutritional screening, distribution of therapeutic food and targeted food distributions to families with malnourished children (millet, beans, oil and sardines). They also distributed jerry cans, soap and mosquito nets and provided outpatient medical treatment and seasonal malaria chemoprophylaxis.
Damboa
In Damboa, southern Borno State, the population is currently estimated at 88,000, with many of them being displaced from the surrounding area. More than 8,600 displaced people live in three makeshift camps in public buildings and the general hospital. Half of the town is destroyed. While food availability has improved and food distributions have started, there is hope that this major concern, especially for IDPs without financial means, will be addressed. There is still insecurity in the direct surroundings and groups of displaced people continue to arrive regularly. From 12 October to 2 November, 681 newly displaced people arrived and arrivals are still being registered.
MSF currently has three clinics providing primarily healthcare and nutrition services, including an ITFC and a paediatric department (with 40 beds altogether), outpatient departments and three ATFCs for severely and moderately malnourished children under five years of age (with more than 420 children currently enrolled in the programme). The number of patients consulted is currently 2,200 per week. The majority of patients have presented with malaria, respiratory tract infections and gastrointestinal problems. Malaria remains the main cause of death in the clinics. The team has set up three community malaria points (‘fever clinics’) within the town, where people with fever can be quickly tested and receive basic treatment. MSF is also running an outreach program with 40 staff members who go through the camps and the town, screen children for malnutrition, bring sick patients to the clinics and distribute therapeutic food to families with small children. The teams vaccinated more than 21,000 children against measles in August, distributed mosquito nets, blankets, soap, buckets, potties, cups and kettles to 14,000 families, provided clean drinking water and built latrines in the camps.
Kaga LGA – Benisheikh
In Kaga local government area (LGA), located in western Borno state, MSF is currently running three ATFCs, located in Benisheikh, the capital town of the LGA, Ngamdu and Mainok. Since the end of September, malnourished children who need to be hospitalised from these three locations are referred to a newly created ITFC in Benisheikh. Before that, all the children requiring hospitalis
ation were referred by MSF teams to the ITFC in Damaturu in Yobe state, also run by MSF. From April to September, a total of 418 kids were admitted to the ITFC in Damaturu; in the ATFC in Benisheikh, a total of 1,098 children were enrolled in the programme from August to September. At the same time, a paediatric ward was opened. Both facilities have 25 beds altogether and we are planning to increase the number of beds. Malaria and malnutrition cases have been increasing in recent days with 263 children treated for malaria from August to September. An additional maternity is planned. The team has recently witnessed new arrivals in Benisheikh.

Gwoza
Gwoza is an isolated, severely damaged town in eastern Borno State. Access by MSF teams is only possible by helicopter. In recent days, the number of new arrivals has already increased a bit. Around 45,000 IDPs are living in the last buildings that have not been destroyed – the school and the so-called ‘20 houses square’. There had been no food distributions for three months prior to the arrival of MSF teams. The IDPs allowed to farm only in the morning, on a specific area on the outskirts of the town.
The MSF team rehabilitated a building to be used as health facility, opened an ITFC and ATFC and are running an outpatient department together with UNICEF. In the first two weeks of activities in October, a total of 238 kids were admitted to the ATFC and 13 to the ITFC. A total of 1,042 patients with malaria were treated and more than the 50 per cent of children tested for malaria test positive. The team also plans to improve access to drinking water – there are some privately-owned boreholes in the town, but the IDPs have to pay for the water. Teams registered a high rate of malnutrition during their assessment in August.
Pulka
Pulka is a town 22 kilometres north of Gwoza, with a current population of at least 30,000 people. Access to Pulka by MSF teams is currently possible only by helicopter. On 22 October, an MSF team started activities in the town. The aim is to set up an OPD, ITFC and an ATFC. No other health actors are currently present in Pulka.
Banki
MSF teams from Cameroon have been providing emergency medical assistance and delivering food in Banki, Nigeria, since July. The town has an estimated population of over 20,000 and most of them are displaced. People are stranded in camp controlled by the military and local defence groups, making them utterly reliant on external assistance for food, water and healthcare. MSF medical teams regularly cross the Cameroon-Nigeria border to provide assistance. Fourteen per cent of the children screened by MSF on 19 July were suffering from severe acute malnutrition, and nearly one in three children was malnourished.
Since July, MSF teams have vaccinated 7,500 children under five against measles and provided preventive malaria treatment to over 7,000 children. MSF also conducted over 1,100 consultations for severely malnourished children, nearly 600 consultations for moderately malnourished children and 195 consultations for pregnant women. Seventy-five tons of therapeutic food have been distributed to malnourished children and some 2,400 families have received food rations in a general food distribution. MSF teams carried out water and sanitation activities in the camp by installing water tanks and generators, rehabilitating boreholes and constructing 32 latrines. The camp residents now have access to 15 litres of drinking water per person per day, compared to just five litres in July.
Mortality rates in Banki were very high. When MSF teams first arrived there in July, a rapid assessment found mortality rates four times the emergency threshold. Since then, the situation has somewhat improved as more assistance started to reach the population. Another survey carried out by MSF in September showed that 70 out of 2,134 children under the age of five died between 20 July and September. Of 8,396 adults, 145 died during the same period. A more recent survey from 16 September to 28 October showed that 14 out of 1,916 children under five died. While this shows that the situation is starting to improve, the mortality rates are still worrying and close to the emergency threshold.
Ngala and Gambaru
MSF teams from Cameroon also provide assistance in Ngala and Gambaru in northeast Nigeria. They managed to reach Ngala for the first time on 19 September, where they found 80,000 IDPs living in a camp in acute need of food, healthcare and clean water – surviving with less than a litre of water per person per day. A rapid nutritional screening of more than 7,000 children under the age of five found that one in ten were suffering from severe acute malnutrition and nearly one in four were malnourished. MSF improved the water supply system by drilling boreholes and rehabilitating water pumps and people now have access to eight litres of water per person per day.
In Gambaru, a town a few kilometres from Ngala, the town’s 55,000 residents lack basic food supplies and have no access to healthcare. The only health centre was burnt down, and the road is too dangerous for people to leave to seek care elsewhere.
On 12 October, MSF teams went back to Ngala and Gambaru. They vaccinated 15,000 children under five against measles and distributed food and relief items to 14,600 families. Teams also treated some 700 severely malnourished children and nearly 4,000 who were suffering from moderate malnutrition. 400 general outpatient consultations were also carried out.





