56,000
56,
4,330
4,33
2,330
2,33

2,100
2,1
1,360
1,36
560
56
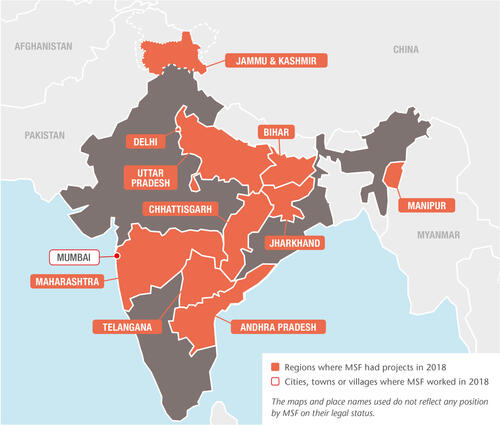
Médecins Sans Frontières (MSF) continues to work in India with vulnerable communities, providing medical care linked to infectious diseases, mental health, sexual violence and malnutrition.
Treating drug-resistant tuberculosis (DR-TB) and HIV in Mumbai
Mumbai’s M East ward is one of the areas with the highest rates of TB in India’s most populous city. For the last 10 years, MSF has worked in an independent clinic that offers comprehensive care for HIV and DR-TB patients – including those with very complex drug resistance patterns that require treatments not available elsewhere in the public or private sector.
In collaboration with the national TB programme and the local government, we also run an outpatient TB department at Shatabdi hospital in M East ward. Many of our TB patients have developed resistance because they have been receiving ineffective treatment for years; others are directly infected by extensively resistant strains. Our model of care provides less toxic and more effective treatments for DR-TB, using newer drugs and offering psychosocial assistance to improve adherence to treatment.
Our teams work in the community to strengthen case finding and adherence to treatment. In 2018, we launched an initiative to ensure systematic clinical and psychosocial follow-up of DR-TB patients at seven health posts, with the objective of demonstrating a replicable model of community-based care.
Specialised care for TB, HIV and hepatitis C in Manipur
Manipur has a high prevalence of HIV, hepatitis C and both drug-sensitive and drug-resistant TB. Due to a lack of healthcare resources, it also has a high incidence of co-infection, which means each disease speeds up the progress of the other, making patients more vulnerable and treatment more difficult.
Through clinics in Churachandpur, Chakpikarong and Moreh, near the Myanmar border, our teams offer screening, diagnosis and treatment, as well as counselling and health education about how to get tested and treated.
In 2018, we increased our support to Churachandpur district hospital, to improve treatment for HIV patients co-infected with hepatitis C. We also started using bedaquiline to treat patients with extensively drug-resistant TB.
Hepatitis C project in Meerut, Uttar Pradesh
Western Uttar Pradesh has a very high prevalence of hepatitis C, a potentially fatal disease that can lead to liver failure and liver cancer if left untreated. We have been running a pilot hepatitis C project in Meerut since January 2017, in collaboration with the National Health Mission.
The aim is to demonstrate the effectiveness of decentralised and simplified hepatitis C treatment and care, and to share best practices for replicating the model in other high-prevalence areas. We provide testing, treatment, health education and counselling at a district hospital.

Fighting kala azar and advanced HIV in Bihar
Kala azar (visceral leishmaniasis) is a neglected tropical disease that is prevalent in Bihar, and co-infection with HIV is a growing public health concern. More than 80 per cent of co-infected patients present with late-stage HIV, often suffering from TB in addition.
Together with the Indian Council of Medical Research and the National Vector Borne Disease Control Programme, we have been developing and implementing more tailored, safe and effective treatments for co-infected patients, and looking for better detection methods to improve their prospects.
Additionally, together with state authorities, we have agreed to set up an integrated centre that will offer holistic care and treatment to patients with advanced HIV, including diagnosis and management of opportunistic infections. The centre, which is due to open in February 2019, will provide a wide range of services, including psychological, nutritional, medical and, where necessary, palliative care.
Mental healthcare in Jammu and Kashmir
Years of conflict have taken a psychological toll on the residents of Jammu and Kashmir, the effects of which are compounded by the stigma associated with mental health issues. We have been offering counselling services there since 2001, and in 2018 had teams working in hospitals in four districts – Srinagar, Baramulla, Pulwama and Bandipora. In Bandipora, we are helping the government to implement a mental health programme with a strong community awareness-raising component.
Sexual and gender-based violence in Delhi
In 2015, we opened a 24-hour clinic in North Delhi’s Jahangirpuri district for victims of sexual and domestic violence. Services include post-exposure prophylaxis to prevent HIV/AIDS, the prevention and management of unwanted pregnancies and sexually transmitted diseases, and psychosocial support. We also run counselling services at the local district hospital.
Throughout 2018, we continued to work with community-based organisations, police, government protection agencies and the health ministry to raise awareness of the clinic’s services and develop an efficient referral system.

Reaching remote communities in Andhra Pradesh, Chhattisgarh and Telangana
A low-intensity but longstanding conflict has left large sections of the population of Andhra Pradesh, Chhattisgarh and Telangana states without access to healthcare. Medical facilities are few and far between, meaning that even preventable, treatable conditions can become life-threatening.
We run mobile clinics to take primary healthcare to remote communities in these states. As well as treatment for malaria, respiratory infections, pneumonia and skin diseases, we conduct health education sessions on topics such as hygiene, care of newborns, family planning and prevention of sexually transmitted diseases.
Treating severe acute malnutrition in Jharkhand
We have been working with the health authorities in Jharkhand to identify and treat children with severe acute malnutrition since 2017. In 2018, we continued to focus on preventive and therapeutic measures, including screening and community engagement.
Together with the Rajendra Institute of Medical Sciences, we launched a study in November to investigate how childhood malnutrition evolves into severe forms, and how it can be addressed most effectively. The results will be shared with policy makers in India, to ensure that in a country with the highest worldwide burden of severe acute malnutrition, children receive the best possible treatment.