August 2018 update on activities in Cox's Bazar district, Bangladesh, providing care for Rohingya refugees who have fled Myanmar.
Summary
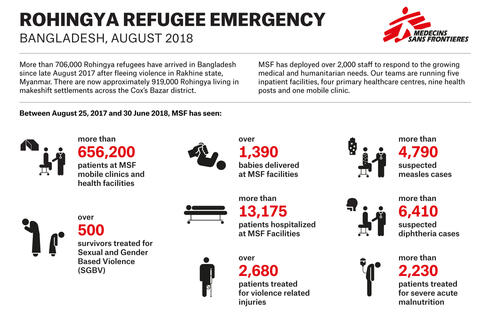
Number of health facilities: 5 inpatient health facilities, 4 primary health centres, 9 health posts/outpatient facilities and 1 mobile clinic (details below).
Number of staff: More than 2,000 MSF staff and over 1,000 volunteers are working to respond to the health and water and sanitation needs of the Rohingya refugees.
Number of patients: Between August 2017 and the end of June 2018, our teams carried out 656,228 outpatient consultations, including over 8,000 consultations for local people living around our health facilities, and 13,115 inpatient consultations.
Main morbidities: Respiratory infections, diarrheal diseases and skin diseases, all related to poor living conditions, as well as non-communicable diseases.
Water and sanitation: Activities include drilling boreholes and tube wells, setting up water distribution systems, trucking in water, desludging old latrines, constructing new sustainable latrines, doing bucket chlorination and distributing domestic water filters.
Mental health services: Mental health services have been scaled up and are now available at most MSF facilities.
Outreach: Outreach teams focus on health promotion, outbreak prevention, alert and response, while surveillance teams gathers demographic, nutritional, mortality and birth indicators, covering 80% of the refugee settlements. An all-female team spreads messages about sexual and reproductive health in the community.
Recent developments
Rainy season
Monsoon season has arrived and intense rains have caused havoc in the camps and for local communities. The rains have resulted in landslides, floods, and fires, which have led to injuries, deaths and destruction of infrastructure and facilities. Some roads have become inaccessible and require extensive repairs.
The Rohingya living in the camps remain at risk of disease outbreaks, aid disruptions and poor or complicated access to healthcare. Since 11 May, over 49,000 people have been affected by at least 560 incidents. These include 297 landslides, which affected over 15,000 people, and 41 instances of flooding, which affected 1,300 households. The monsoon season is expected to last from June to September.
Relocations
Even as the rain falls, thousands of people in the Kutupalong-Balukhali and Nayapara camps continue to be relocated due to unsustainable and dangerous conditions. In Kutupalong-Balukhali, people are moved to the western edge of the camp where there is a lack of basic services.
Initially, these new locations were hastily prepared and often inadequate. Emergency shelters were sometimes located on the edge of subsiding land, water provision and sanitation were insufficient, and many health structures were not yet operational. This left thousands of people in a dire situation during some of the heaviest days of rain.
Since mid-June, organisations responsible for relocations have made noticeable progress on improving the new destination camps and efforts have been made to consult communities prior to moving them. In spite of ongoing relocations, tens of thousands of Rohingya in the district are directly at risk due to landslides and flooding, which can also cause overflowing toilets and the contamination of drinking water.
Living conditions
Overcrowding and congestion continue to be of major concern. The Kutupalong-Balukhali expansion site continues to expand to the west, where the land consists of remote, hilly terrain that has been stripped of trees and vegetation. This is also a concern in Nayapara, the main refugee site in the south of the peninsula. While additional land is being prepared, not enough suitable land has been made available by the Bangladesh authorities to relocate all those who are affected away from high risk zones.
Access to safe drinking water and sanitation services is insufficient in the existing camps and in particular in new camps along the western edge of the Kutupalong-Balukhali expansion site, which increases the vulnerability of the people living there. Without adequate access to water, sanitation and hygiene, communicable disease outbreaks are likely to occur.
Fewer but continued arrivals
The number of Rohingya people arriving in Bangladesh from Rakhine state has steadily decreased over the past few months but those arriving tell MSF teams that incidents of violence, harassment and detention continue, as do household checks and coerced registration for the National Verification Card (NVC).
As of mid-June, the UNHCR had recorded over 11,000 new arrivals in Bangladesh since the start of 2018, the majority of whom arrived during the first three months of the year.
The presence of such a huge refugee population has put immense strain on the Bangladeshi host population. Tensions are exacerbated by existing levels of poverty in Cox’s Bazar, high population density and vulnerability to natural disasters.
‘No man’s land’
A group of about 4,200 Rohingya have been living in the so-called no man’s land on the border between Myanmar and Bangladesh since the end of August 2017. The Rohingya in the no man’s land report being frequently threatened and harassed by the Myanmar military, including through the use of loudspeakers. A number of incidents have taken place in the area, the latest on 28 June, when a young child was shot in the leg while playing near the fence on the Myanmar side.

Current health concerns
The health concerns among Rohingya refugees remain fairly consistent. The main health issues continue to be related to poor living conditions, including respiratory tract infections, diarrheal diseases and skin diseases.
MSF has set up several diarrhoea treatment units/centres in order to be ready to respond to a possible increase in cases of acute watery diarrhoea. Mental health and sexual and gender-based violence also continue to be of concern.
We continue to monitor health indicators and incidents through outbreak and surveillance systems and are prepared to respond, including setting up several diarrhoea treatment facilities.
We are seeing fewer diphtheria cases, with an average of 44 cases per week in July, compared with an average of 178 cases per week in January and February.
Monsoon season
The monsoon season has brought landslides and flooding, which put people at increased risk of traumatic injuries. Several people have been treated for injuries related to landslides, and MSF teams have seen cases of drowning, particularly among children and the elderly. Flooding also leads to greater risk of waterborne diseases, which could cause epidemic outbreaks.

How the monsoon affects Rohingya refugees
Vaccination coverage
There is also a focus on vaccinations as the majority of the Rohingya had extremely low immunisation coverage as a result of decades of restricted access to healthcare in Myanmar. Over the past few months, cholera, diphtheria and measles vaccination campaigns have been carried out but routine vaccination levels are still relatively low. MSF provides routine vaccinations at most of our health facilities, in partnership with the local authorities.
Mental health
The targeted violence that forced Rohingya refugees to flee their homes in Myanmar, combined with the hazardous journey and the daily stresses of life in the camps, means that many refugees experience flashbacks, generalised anxiety, panic attacks, recurring nightmares and insomnia, as well as illnesses such as post-traumatic stress disorder and major depression. We are also seeing more chronic mental health difficulties and psychiatric needs.
Some of the factors that contribute to people’s distress include a lack of sufficient food, a lack of opportunities to make a living, restrictions on freedom of movement beyond the camps and fears for personal security within the camps. This is further exacerbated by insecurity concerning their future and a lack of decision-making power and control over their own lives.
As well as providing mental health services to Rohingya refugees, a significant portion of MSF’s mental health activities serve local communities around the refugee settlements, ensuring that the mental health needs of the host population are also addressed.
Sexual and gender-based violence
MSF teams also continue to provide services for victims of sexual and gender-based violence (SGBV). Rates of intimate partner and domestic violence are high.
Intimate partner violence is often driven by a range of factors including pre-existing gender inequalities, and exacerbated by rapidly changing gender roles triggered by displacement, additional stresses due to loss of livelihood, and isolation from community and family support systems. These factors are further intensified by trauma sustained through violent experiences.
More needs to be done to ensure that protection and services specifically designed to meet their needs are available to the most vulnerable among the Rohingya refugees.
Water and sanitation
MSF’s water and sanitation response focuses on improving access to clean, treated water and servicing/maintaining existing infrastructure such as latrines, showers and tube wells.
Sanitation
Monsoon rains and resulting landslides and flooding have damaged and even destroyed latrines. Some have collapsed; others have rapidly filled up and begun to overflow. MSF teams continue to monitor the situation and have begun constructing a facility to safely process waste from latrines.
Clean water
The biggest concern with regard to clean water is contamination at household level. Between March and July 2018 , more than 9,000 water samples were collected for bacteriological testing. This testing showed overwhelmingly that the major source of bacteriological contamination was occurring during collection, transit, storage and usage of water at the household level, with some 46.5 per cent of tested samples at household level showing e-coli contamination.
MSF continues to provide water to households and distribute household aqua-filters (bucket water filters). These water filters are distributed as a preventive measure in areas where outbreaks of waterborne diseases are suspected and to MSF patients when they are discharged.
To date, MSF has drilled 12 productive boreholes and 362 tube wells with hand pumps. “Bucket chlorination” – providing chlorine to treat water at the point where water is collected – also continues, particularly in areas where water quality and sanitary conditions are poor and/or there is a particular risk of outbreaks.
The data from the tests mentioned above, however, overwhelmingly supports the needs for centralised treated water supply strategy as the only way to protect water during the transit and storage phases as a key requirement to prevent outbreak. In order to support this, MSF is working to set up water distribution systems that will reach more people, including gravity-fed and other distribution systems.
Two water distribution systems have been constructed and additional new projects are currently ongoing, planned for completion in the next few months.
Outreach and outbreak monitoring teams track incidents related to water and sanitation. Water quality is also monitored regularly.
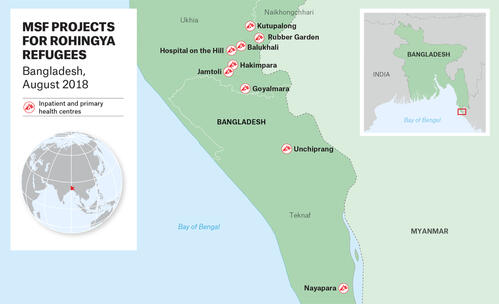
MSF project locations
MSF teams are providing a wide range of health services for Rohingya refugees living in formal and informal camps, as well as for the local host population around our facilities. MSF’s projects serving Rohingya refugees and local host communities are located along a peninsula between the Bay of Bengal and the border with Myanmar, in southeastern Bangladesh. The distance from Cox’s Bazar town to Sabrang entry point (border post) is approximately 100 kilometres.
Cox's Bazar town
- Project working on infection prevention and control improvement at district hospital
Kutupalong-Balukhali mega-camp (over 600,000 refugees)
- 3 hospital-level inpatient facilities (Kutupalong, Balukhali and Hospital on the Hill)
- 8 health posts/outpatient facilities
- Surveillance and outreach activities, including health education, referrals and collecting demographic, nutritional, mortality and birth indicators
- Water and sanitation activities, including drilling boreholes and pipe wells, bucket chlorination, distribution of household aqua-filters and building water-distribution systems
- Rubber Garden diphtheria treatment centre and new acute watery diarrhoea treatment centre
- Rapid medical intervention team for emergency response
- Mobile clinics can be activated if the need arises
Hakimpara, Jamtoli and Moynarghona camps (over 100,000 refugees)
- 1 hospital-level inpatient facility (Goyalmara hospital, just outside the camps, also serving the “host” community)
- 2 primary health centres
- 1 health post/outpatient facility
- Surveillance and outreach activities, including health education, referrals and collecting demographic, nutritional, mortality and birth indicators
- 2 additional health posts planned in Jamtoli camp
Unchiprang camp (23,000 refugees)
- 1 primary health centre with diarrhoea treatment centre
Nayapara camp (100,000 refugees)
- 1 primary health centre with diarrhoea treatment centre
Sabrang entry point (border crossing)
- 1 mobile clinic in case of a new influx of refugees
MSF health facilities and services
Inpatient facilities (hospital-level facilities)
MSF operates four hospital-level inpatient facilities in the Cox’s Bazar district and one inpatient outbreak response centre (Rubber Garden).
The four hospital-level facilities offer a range of services including:
- 24-hour emergency services and ambulance referral,
- Inpatient and outpatient departments,
- Sexual and reproductive health services,
- Maternity, neonatal and paediatric facilities,
- Isolation beds/wards,
- Mental health services,
- Sexual and gender violence services, and
- Laboratory services.
Three of the five inpatient facilities are located in the Kutupalong-Balukhali mega-camp, which is home to more than 600,000 refugees, while Goyalmara hospital is located between the Moynarghona and Unchiprang camps. The Goyalmara and Kutupalong inpatient facilities are located outside of the camps and serve both camp and “host” populations. Balukhali hospital has a particular focus on maternal and child health, while the Hospital on the Hill recently introduced a programme to address non-communicable diseases such as hypertension and diabetes.
Both the Balukhali and Goyalmara facilities acted as diphtheria treatment centres at the height of the outbreak. Diphtheria cases are now referred to MSF’s Rubber Garden facility. The Rubber Garden multi-outbreak response centre is an inpatient facility specifically providing treatment in the event of an outbreak and is involved in active case-finding, contact tracing and follow-up.
MSF also has a project at the Sadar district hospital in Cox’s Bazar town. This 250-bed hospital is run by the Ministry of Health and Family Welfare. It manages around 500 patients per day, mostly from the local community. MSF is working on upgrading the infection prevention and control (IPC) facilities and systems at the hospital, including training staff and providing all materials to implement improved protocols. A new waste area and a new laundry room for high-risk linen (from surgery and maternity departments) will be constructed in the coming months and the external grey water system will be rehabilitated.
Primary health centres
MSF operates four primary health centres (PHCs) in the refugee camps towards the south of the Cox’s Bazar peninsula (in Hakimpara, Jamtoli, Unchiprang and Nayapara camps).
These PHCs are outpatient facilities that provide key emergency, primary health and referral services, including:
- 24-hour emergency room and ambulance referral system,
- Outpatient consultations,
- Mental health services,
- Sexual and reproductive health services, including antenatal, delivery and postnatal care,
- Sexual and gender based violence services,
- Vaccinations, dressing rooms, and rapid diagnostic tests.
Each of these PHCs sees between 180 and 300 patients per day. Outreach teams working with PHCs focus on health promotion, community referral for potential outbreak alert and response, while surveillance teams gather demographic, nutritional, mortality and birth indicators.
Unchiprang PHC has a diarrhoea treatment unit, with a capacity of 40 beds, which can be activated in the event of an outbreak. MSF is also setting up a 100-bed diarrhoea treatment centre at Nayapara PHC.
Health posts and mobile clinic
MSF runs nine health posts (eight in Kutupalong-Balukhali and one in Moynarghona), and one mobile clinic at Sabrang entry point (border crossing).
The health posts in Kutupalong-Balukhali offer different services, including outpatient consultations, vaccinations, follow-up of non-communicable diseases (NCDs), sexual and reproductive services (antenatal, postnatal, sexual and gender-based violence and family planning), and mental health services. Moynarghona health post also operates a 24-hour ambulance referral system.
MSF’s mobile clinic has been working to provide screening, consultation and referral services to newly arrived refugees and the host population around the Sabrang entry point (border crossing). As the number of new arrivals has now decreased, this mobile clinic has been put on standby. An MSF social worker continues to provide daily follow-up and monitor the situation, so that the mobile service can be quickly reactivated if needed.







