10,900
10,9
1,000
1,
280
28

680
68
Swaziland has one of the world’s highest rates of HIV, affecting roughly one in three adults. The HIV epidemic is showing signs of stabilising and in recent years the number of AIDS-related deaths has reduced. Based on a 2017 HIV incidence survey, the rate of new infections has almost halved within five years.
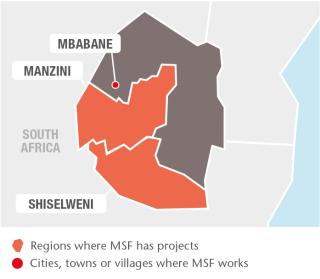
In Shiselweni region, MSF continued with its ‘test and treat’ strategy, providing immediate treatment at the time of HIV diagnosis, irrespective of clinical criteria. In addition, MSF introduced innovative approaches such as pre-exposure prophylaxis (PrEP) for patients at increased risk of HIV infection, and oral HIV self-testing for hard-to-reach people. A total of 129 patients initiated PrEP and 2,140 people have accessed HIV self-testing since May.
MSF is increasingly focused on providing specialised care and support for people living with HIV. This includes providing second- and third-line antiretroviral (ARV) treatment, cervical cancer screening and routine point-of-care screening for the cryptococcal antigen, an indicator of meningitis. In 2017, 2,637 women were screened for cervical cancer, 17 per cent of whom tested positive. Of these, 60 per cent were treated. MSF also provides community-based HIV care, including treatment clubs for adults and children.
Swaziland has one of the highest TB notification rates worldwide. Because of the close connection between the HIV and TB epidemics, 70 per cent of people who contract TB are also HIV positive.
In Manzini region, MSF continued its research into the shorter-course treatment for multidrug-resistant TB (MDR-TB). A total of 149 patients were enrolled in the study; 132 patients finished their treatment, with a cure rate of 72 per cent. The study will be concluded in 2018 when the one-year follow-up is finalised. Since 2017, the shorter DR-TB regimen has been included in the national protocol, with MSF providing technical support for its implementation.
MSF continued to offer technical support to the national TB reference laboratory in Mbabane and helped to upgrade the Bio Safety level 3 laboratory.
The national TB programme has made significant progress with regards to provision and use of new TB drugs, diagnostics and decentralisation of treatment and care. It also started taking over the provision of support packages for DR-TB patients. These include nutrition and treatment support, as well as transport costs, which help improve patients’ adherence to their regimen.
Due to the decreased incidences of HIV and TB, the resulting lower illness and mortality rates, and improvements in the Ministry of Health’s capacity to manage the diseases, MSF has decided to gradually hand over its projects in Manzini. In March, MSF handed over most of its services at Matsapha comprehensive healthcare clinic to AIDS Healthcare Foundation, while continuing to support the DR-TB programme and the laboratory. In December, DR-TB activities in Mankayane hospital and Luyengo clinic were handed over to the Ministry of Health.