1,772,000
1,772,
856,500
856,5
122,800
122,8

42,700
42,7
38,300
38,3
19,200
19,2

15,800
15,8
7,300
7,3
4,700
4,7
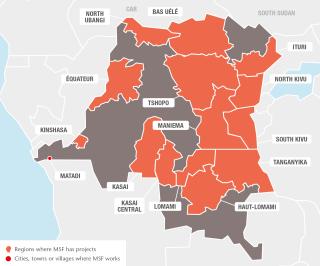
Millions of people were displaced in the DRC in 2017 as new waves of violence erupted.
Conflict in Tanganyika province has intensified over the last couple of years, which has led to the displacement of over half a million people. In 2017, MSF stepped up its response, providing emergency assistance in Nyunzu and in makeshift camps in Kalemie and the surrounding areas. Many of the displaced are living in and around the town of Kalemie with host families, in makeshift camps or in school compounds. Some are sleeping on the ground with only a mosquito net for shelter. MSF activities included measles vaccinations, mobile clinics offering primary healthcare, as well as reproductive health services and mental health consultations, support to health centres and paediatric inpatient care. Teams also distributed water and built latrines and showers in some of the camps.
More than 1.3 million people fled extreme violence in Greater Kasai region, with some escaping into the bush and hiding for weeks despite dire medical needs, unable to access care due to insecurity. MSF teams were able to treat some who had suffered severe injuries such as deep machete or gunshot wounds. The conflict triggered an acute nutrition crisis in rural areas and a sharp increase in sexual violence. Teams treated war-wounded patients in a rehabilitated wing of Kananga city hospital, performing 1,204 surgical interventions and provided care for victims of sexual violence. In Tshikapa, MSF supported care in a hospital, three health centres and the prison. On the outskirts of both cities, where many of the health centres had been looted, destroyed or burned, MSF ran mobile clinics.
Assistance for refugees and host communities
In September, MSF started to assist people who had fled conflict in Central African Republic by supporting hospitals in the northern towns of Gbadolite and Mobayi-Mbongo. Mobile clinics also provided care to some 67,400 refugees and their host communities.
Tens of thousands of South Sudanese refugees have settled in the north of DRC. MSF ran mobile clinics in the villages of Karagba and Olendere, in Ituri province, offering refugees and host communities access to basic healthcare, mental health support, sexual and reproductive health consultations, and referrals. A team also supported the regional hospital.

Providing comprehensive care in the Kivu provinces
The Kivu provinces are still reeling from the devastating Congo Wars of the 1990s and are plagued by ongoing fighting. More than 1.5 million internally displaced people live in the Kivus, where the humanitarian and medical needs only intensified in 2017 as the situation in the provinces deteriorated. Overall, MSF provided almost 1.5 million outpatient consultations and admitted more than 95,000 patients to its facilities in North and South Kivu.
Teams continued to manage four comprehensive projects in Masisi, Walikale, Mweso and Rutshuru in North Kivu. Each supported a hospital, as well as health centres and community treatment sites. A new project was also set up in Bambo.
When violence broke out again in South Kivu in July, MSF treated the wounded, while continuing with its regular activities. In Lulingu, Kalehe and Mulungu, the team focuses on care for children under 15, sexual and reproductive healthcare and treatment for victims of violence. Teams also implement a community-based approach to treat malaria and malnutrition. The main activities in Baraka and Kimbi are paediatric care, HIV and tuberculosis (TB) treatment, sexual and reproductive health, and care for victims of sexual violence.
Response to epidemics
Due to poor access to healthcare, the average life expectancy in DRC is around 58 years. One in 10 Congolese children dies before the age of five.
Emergency response is a core activity for MSF in the country. Five teams are dedicated to monitoring health alerts and deploying a rapid response to outbreaks of violence, population displacement and epidemics across this vast country. In 2017, MSF launched 62 emergency interventions. During the first half of the year, most were in response to multiple measles outbreaks. In total, teams vaccinated 1,050,315 children against measles, and treated 13,906 for the disease.
From mid-2017 MSF switched its focus to a cholera epidemic that started in the Kivus, where cholera is endemic. It spread to the rest of the country, becoming one of the biggest outbreaks in DRC of the last two decades. Overall, MSF cared for 19,239 cholera patients nationwide.
MSF also responded to an Ebola outbreak in remote Likati province in May; four people died during the outbreak, which was quickly contained.

Addressing longstanding health issues
Malaria is endemic and the main cause of death in DRC. MSF teams treated 856,531 patients for the disease in 2017, more than for any other illness. MSF experimented with new models of care that can be adapted to local settings to improve treatment, for example the introduction of large-scale community-based projects. These are currently running in Baraka and Kimbi, and teams in Bili, Mweso and Walikale are exploring this option.
Women’s health remains an important component of most MSF projects. This includes treating patients who have had unsafe abortions and care for people who have suffered sexual and gender-based violence, especially in Kasai, the Kivus and Mambasa in Ituri.
In 2017, MSF intervened in the Kivu provinces, Uélé and Kasai regions to address high levels of malnutrition among children.
MSF continues to provide comprehensive medical and psychosocial care for people living with HIV and AIDS in Kinshasa, Goma, Baraka and Kimbi, and works with the national HIV programme, partner organisations and patient groups to improve access to testing and treatment. In 2017, 7,185 patients received antiretroviral treatment at MSF-supported health centres in Kinshasa, Goma, Mweso, Baraka and Kimbi. Over 2,990 patients with late-stage HIV were treated in MSF’s AIDS unit in Kinshasa alone.
In Maniema province, an MSF mobile team tested over 18,000 people for human African trypanosomiasis, also known as sleeping sickness, 42 of whom required treatment. While the prevalence of this neglected disease has decreased in the past decade, there are still many presumed hotspots that are difficult to access.
Project closures
In March, MSF closed its Shabunda project in South Kivu. In seven years, 927,000 outpatient consultations were carried out. In April, MSF closed the project in Manono, where teams had worked in the regional hospital’s paediatric department and health centres.
At the end of the year, activities in Rutshuru, Boga and Gety were handed over to the Ministry of Health. During its 11 years in Gety, MSF undertook 573,200 outpatient consultations and assisted almost 13,500 births.
Our missing colleagues
On 11 July 2013, four MSF staff were abducted in Kamango, in the east of DRC, where they were carrying out a health assessment. One of them, Chantal, managed to escape in August 2014, but we are still without news of Philippe, Richard and Romy. MSF remains committed to obtaining their liberation, including through the mobilisation of a crisis management team. On 30 September 2017, a member of the crisis management team was sentenced to 10 years’ jail for his involvement in trying to solve the crisis. MSF is working to resolve this situation in the best possible way.
2,881
2,881
101.7 M
101.7M
1977
1977
Patient Story
“We live in a village in Walikale territory. One night I saw armed men in my house – I don’t know how they got in. As soon as I saw them I grabbed my two youngest children and tried to take cover under the bed. My eight-year-old son tried to do the same, but the men shot him. The bullet hit him in the chest and he fell next to the bed, dead.
They fired towards the bed where we were hiding. My two-year-old and four-year-old sons were hit by bullets. I shouted, ‘You’re killing me and all my children’, and they replied, ‘All you have to do is die!’
I walked for an hour with my children to a health post and then the MSF ambulance took us to Masisi general referral hospital where they were treated. They are a bit better now. I hope they can forget about this tragic incident. So far they haven’t talked about it.”
*Patient’s name changed