Over the past decade, Médecins Sans Frontiers (MSF) has shifted its approach to mental health care to integrate it more deliberately in all activities.
Today, mental health care is at the forefront of our projects from Latin America to Africa, to Asia and the Mediterranean Sea, as well as across Europe. In the past 10 years, mental health consultations in our projects have risen by 230 per cent worldwide.
This enormous increase in providing care for mental health illustrates the shift in our approach as well as the diverse and complex psychological needs people face in myriad contexts, from war-wounded and traumatised children in the Middle East, to families fleeing conflict and making perilous journeys across Africa, Central America, and the Mediterranean Sea.

A lack of services
“As there are almost no providers in the contexts where we work, we often have to create our own mental health programmes,” says Marcos Moyano, MSF mental health advisor. “I recently visited our projects in Greece, where we provide specialised mental health support for refugees, migrants and asylum seekers.
“The suffering these people have been exposed to and the level of their mental health needs are amongst the highest we have ever seen. But there are very few organisations who provide specialised care to these people,” says Moyano.
In addition to the lack of services, come taboos, stigmas and suspicion surrounding mental health in many parts of the world. We have to work with communities to spread awareness and educate people on the importance of mental health. Despite the varying challenges, whether providing support in emergencies or treating people affected by war and conflict, treating mental health needs across the world remain a priority for our teams.
The suffering these people have been exposed to and the level of their mental health needs are amongst the highest we have ever seen.Marcos Moyano, MSF mental health advisor
Living under occupation in Palestine
In Palestine, people live under ongoing occupation and regularly experience intense violence. As a result, those forced to live in such conditions often suffer from mental health conditions. People arriving at our clinics present with varying symptoms including sadness, anger, hopelessness, nightmares, bed-wetting and suicidal thoughts.
In Gaza, a counsellor meets regularly with MSF trauma and burn patients and their caretakers to help them heal from their traumatic experiences, ensuring the best chance of recovery. In Hebron and Nablus districts, our teams of psychologists and counsellors carry out individual and group sessions with adults, teenagers, and children.

Mental health in Palestine
“Our life is difficult. All the settlers around are armed,” says Mariam Khdeirat, a resident of Hebron. “My children were walking with the sheep and the soldiers and settlers came to attack them. Some of the settlers were armed and some were with dogs.
“Day and night we feel threatened and afraid. Even when we sit to eat, we are afraid of them,” says Mariam
“We are providing mental health support to the residents of Hebron, but we cannot solve the problem of settler violence against the Palestinian people,” says Salah Daraghmeh, MSF project coordinator in Hebron. “Only the Israeli authorities can do that.”
Day and night we feel threatened and afraid. Even when we sit to eat, we are afraid of them.Mariam Khdeirat, a resident of Hebron
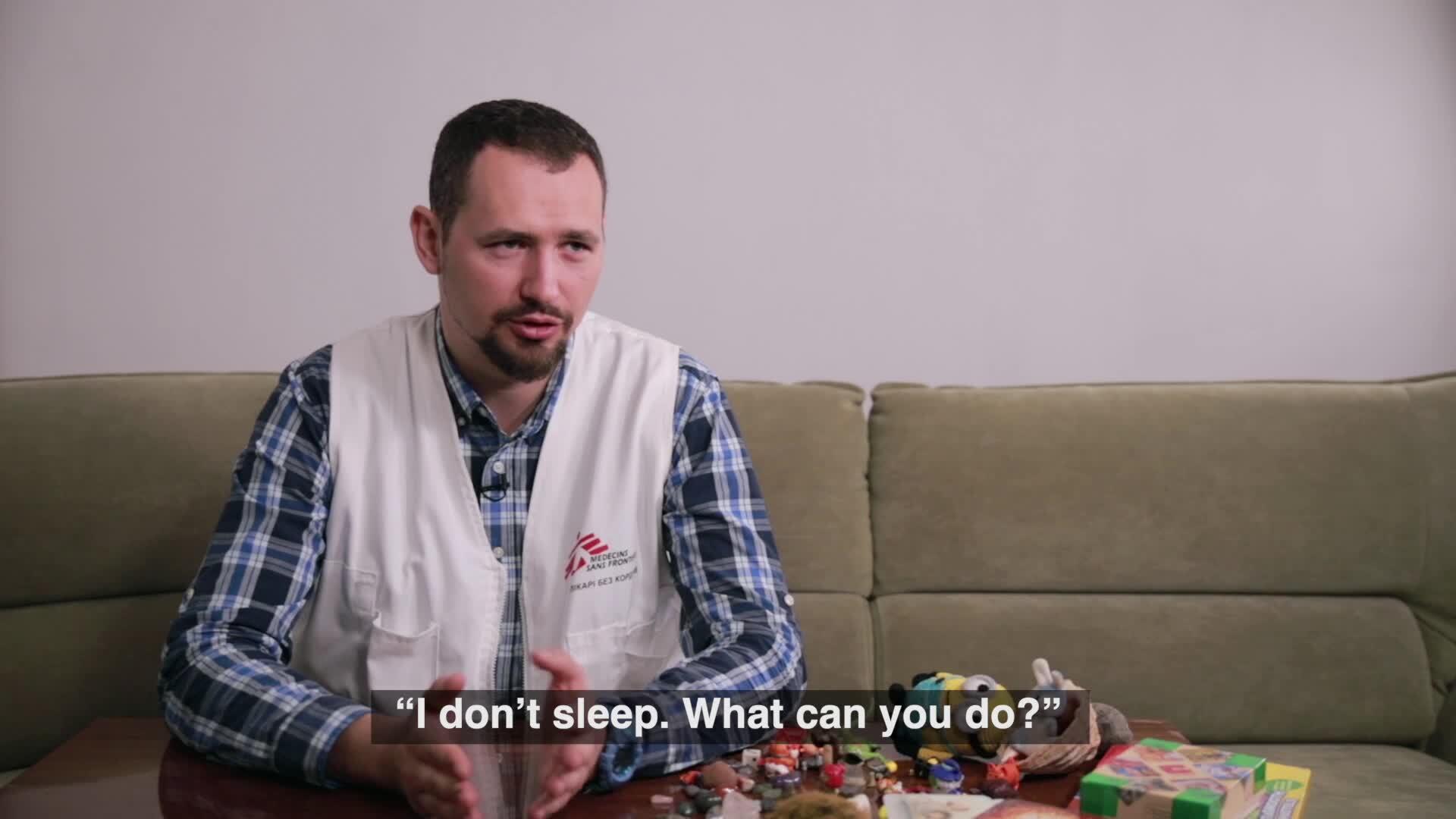
The constant fear of conflict in Ukraine
After seven years of conflict, mental health needs among people in towns and villages near the contact line in eastern Ukraine are worryingly high. Many people have lived with the constant risk of violence since 2014.
The psychological impact of conflict has been going on for a long time. For people still living through it, the trauma – both of the initial fighting and of the ongoing threat of explosions, shooting, bombing and landmines – is part of daily life.
Mental health in conflict
“My daughter was just in front of me, 10 metres away. I was at the doorstep,” says Tetiana Karadzheli, an MSF volunteer in Kamianka village, Donetsk region. “Suddenly, the shooting started. I just remember being hit on the head.
“I woke up [with] my grandson hugging me, ‘Granny, we are alive, we are okay’. That was it – the last drop,” says Tetiana. “I am a strong woman but at that moment, I broke. There are no words to explain it, that feeling of fear. Safety didn’t exist at all.”
Our psychologists, and the doctors and nurses we work with, in eastern Ukraine see many patients struggling with depression, anxiety and other common disorders.
“Most frequently it’s acute stress and grief for the loss of their loved ones and homes. In addition, anxiety-related conditions such as insomnia, are wide-spread,” says Tetiana Azarova, MSF Psychiatrist.
I am a strong woman but at that moment I broke. There are no words to explain it, that feeling of fear. Safety didn’t exist at all.Tetiana Karadzheli, an MSF volunteer in the Donetsk region
People living in small towns and villages often can’t afford to travel to cities or pay private mental health providers, even if they can overcome the stigma associated with mental illness and seek treatment.
Training and supporting family doctors and nurses is an example of the new approaches our teams are implementing to make mental health care services available for conflict-affected communities in eastern Ukraine. However, more support and more programmes like this are needed to ensure that patients are no longer left to suffer in silence.

The evolution of mental health care
“In the last decade, there has been significant progress in terms of awareness of mental health needs and the existent gaps of quality care,” says Moyano.
“Nowadays, governments, donors and the international community are much more sensitive to these aspects,” he says. “With the COVID-19 pandemic, we saw mental health widely recognised as a key aspect of people’s wellbeing.”
However, even though mental health awareness has grown and effective treatments for mental health conditions are available, we know that in low- and middle-income countries, less than 10 per cent of people in need receive adequate treatment.
The resilience of communities and the strength of local organisations and volunteers will play a key role in protecting and supporting those in need.Marcos Moyano, MSF mental health advisor
“In the coming years, I think that we will continue encountering tremendous levels of human suffering linked to man-made and natural disasters that will challenge the capacity of governments and organisations to effectively provide a response,” says Moyano.
“In contrast, the resilience of communities and the strength of local organisations and volunteers will play a key role protecting and supporting those in need.”






