This report – now in its third edition – analyses the sources and prices of medicines used to treat drug-resistant tuberculosis (DR-TB), examines the key factors that shape the access environment for DR-TB medicines, reviews the research and development landscape for DR-TB treatment regimens, and makes recommendations for the way forward to reach more people and improve treatment outcomes.
MSF clinics and The Union TB experts are recording alarming rates of people with drug-resistant forms of TB, not only among patients for whom first-line treatment has failed, but also in patients newly diagnosed with TB – a clear sign that DR-TB is being transmitted from person to person in the communities in which we work.
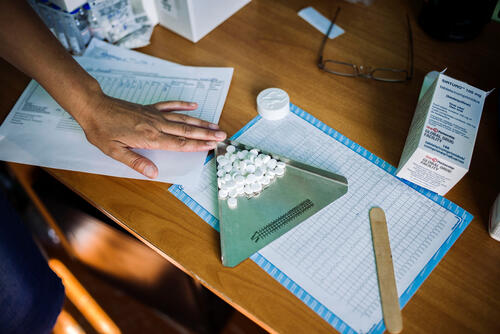
Treatment regimens for drug-resistant forms of the disease, which are more difficult to diagnose and treat than drug-sensitive (DS) TB, are notoriously lengthy, toxic, expensive and burdensome to patients. DR-TB patients must endure about two years of treatment with excruciating side effects, including psychosis, deafness and constant nausea, with painful daily injections for up to eight months. Those who make it through the treatment for multidrug-resistant TB (MDR-TB) only have about a 50% chance of being cured; for extensively drug-resistant (XDR) strains, it’s just 13%.Meanwhile the current recommended treatment course for MDR-TB costs at least $3,000 per patient today, compared to just $22 for drug-sensitive TB treatment.
The utter inadequacy and high costs of today’s current recommended DR-TB treatment regimens contribute directly to abysmally low treatment coverage, which in turn allows drug-resistant forms of the disease to spread rapidly. Inadequately treated patients, poor treatment adherence due to intolerable side effects, poor efficacy and the use of low quality TB medicines are also major contributing factors to the unchecked spread of DR-TB strains. DR-TB represents a serious threat to public health, burdening families and communities with high rates This report – now in its third edition – analyses the sources and prices of medicines used to treat drug-resistant tuberculosis (DR-TB), examines the key factors that shape the access environment for DR-TB medicines, reviews the research and development landscape for DR-TB treatment regimens, and makes recommendations for the way forward to reach more people and improve treatment outcomes. of unnecessary death and sickness, and saddling treatment programmes with much higher costs.
Although far from ideal, today’s current recommended regimens represent one of the few lifelines currently available to people living with DR-TB. Until improved treatment options are widely available, continued use and scale up of the existing treatment regimens must remain a critical component of any strategy to control the DR-TB epidemic.
Today, we’re closer than ever to having more tolerable, all-oral, short-course regimens that, if made widely accessible, could fundamentally transform DR-TB treatment. At the end of 2012, the first new TB drug in 50 years received accelerated approval for use in treating MDR-TB, and a second new drug is currently under review. Many questions remain unanswered about how these new drugs should be incorporated into optimal treatment regimens. A historic opportunity could be squandered amid a lack of collaboration and transparency that is critical to evaluating new multi-drug treatment regimens. Furthermore, meaningful treatment scale up will only occur if these new regimens are made available at prices that are substantially lower than today’s prohibitively expensive options.
In addition, there is growing evidence that repurposed drugs – drugs with indications for diseases other than TB – can significantly improve patient outcomes, particularly for XDR-TB. Unfortunately, these drugs are not yet readily accessible either for further research or to treat patients, and there are many barriers to wider use, including cost, regulatory issues and a lack of incentives for industry to promote access.
Looking further ahead, it is important that the drug pipeline for TB has a range of new candidates in each phase of clinical development, to ensure clinicians can stay ahead of new resistance patterns.
Some of these gaps and barriers may take years to resolve, but in the meantime, governments can and should increase rapid screening and diagnosis of DR-TB, increase access to today’s treatments, and take concrete steps to ensure that new DR-TB drugs are approved, affordable, and available.
Global health actors, including the Global Fund to fight AIDS, Tuberculosis and Malaria and the Global Drug Facility, should act now to mobilise funding, consolidate demand, and ensure a sustainable supply of new and existing effective DR-TB drugs. The world has waited half a century for newer and more effective TB and DR-TB treatments. Now that hope is on the horizon, concerted efforts are needed on all fronts to avoid any further delay in relieving unnecessary pain and suffering for patients and their families, and in permanently turning the tide against DR-TB.