A minor edit was issued for a quote in this article on 2 December 2024.
“I have always been passionate about medicine, but that passion deepened when my mother was diagnosed with diabetes and also contracted HIV,” says HIV specialist Dr Filomena Januário, who works for Médecins Sans Frontières (MSF) in northern Mozambique.
Fearful of other people’s judgement, her mother did not seek treatment for HIV and eventually died from complications associated with the disease.
“She struggled to accept her diagnosis and, sadly, she eventually lost her life,” says Dr Januário. “That loss became my turning point. I promised myself: I will change this reality. I will dedicate my life to health so that I can care for my own family. Maybe if I had been a doctor [at the time], my mother’s life could have been saved.”

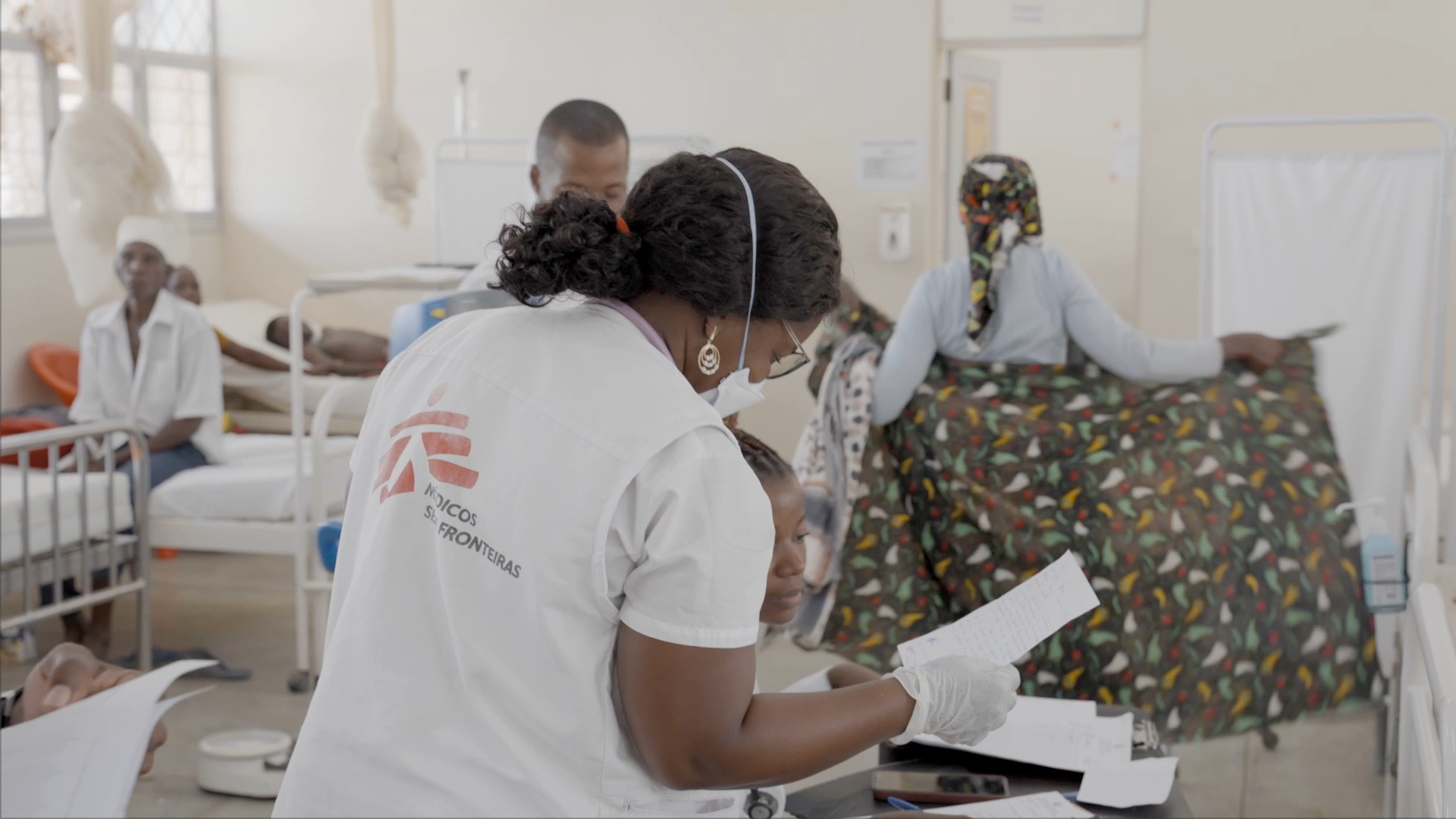
Dr Januário’s commitment to tackling HIV is deeply personal. Through her work at the rural hospital in Mocímboa da Praia, Cabo Delgado province, she strives to ensure that no one else faces the same barriers her mother did to receiving lifesaving HIV care.
Mozambique faces one of the highest HIV prevalence rates in the world; 11.5 per cent of adults and children aged between 15 and 49 live with the virus. More than two million people are currently receiving antiretroviral treatment, which has been instrumental in reducing HIV-related transmission and deaths. However, many challenges persist, particularly in provinces like Cabo Delgado, where armed conflict has disrupted people’s access to medical care since 2017.
Conflict and displacement
Ongoing violence in Cabo Delgado province has forced thousands of people to flee their homes. Many live in precarious conditions, with inadequate shelter, too little to eat and poor sanitation – factors that exacerbate their vulnerability to infections, particularly for those people whose immune systems are already weakened by HIV.
Even when HIV care is available, stigma and discrimination deter many people from seeking treatment. For those who are on treatment, a lack of integrated care can make it hard for patients to stick to their medications, which needs to be taken daily.

“One day, a patient is treated here, and the next day in another hospital, so the care is not integrated,” says Dr Januário. “Many don't have a healthcare card, don’t know what medication they were taking, or how long they had been taking it.”
Since 2019 MSF has been working to bolster medical care and humanitarian aid for people in Cabo Delgado province. Working in partnership with the local Ministry of Health, MSF deploys medical staff, donates medications, and offers mental health support.
One focus of MSF’s work in Cabo Delgado is HIV care, which poses two major challenges, according to Dr Januário: ensuring consistent follow-up care for patients displaced from their homes by violence and addressing stigma within the community.
“[Typically, patients] come to us because they relapsed,” says Dr Janúario. “We treat them, stabilise them and restart their antiretroviral treatment, but we don't know if they return to their place of origin or not. These patients are rarely retained in the programme. Once in the advanced stages of HIV, patients without continuous treatment progress are more susceptible to stage-three and stage-four [major] infections.”
A mentor for expectant and new mothers
Working alongside Dr Janúario is Cristina Virgílio, a mãe mentora (mothers’ mentor), who plays a vital role in preventing mother-to-child transmission of HIV. Cristina runs awareness sessions for HIV-positive pregnant women and new mothers, encouraging them to seek support and stay on treatment.
Cristina herself lives with HIV and is a positive role model for the women, showing them that it is possible to bring up a family and live a healthy and happy life with the virus. Through this peer-to-peer approach supported by the Mozambican Ministry of Health, she helps build trust and dispel misconceptions about HIV, fostering a more inclusive and informed community.

“At first, when you receive the diagnosis, it can be hard,” say Cristina. “It’s important to support the person, reassure them and show that this is not the end of the world. I’ve been living with HIV for many years. I’ve been taking my medication regularly and nothing serious has happened.”
“I have children who were born healthy,” says Cristina. “For example, my daughter is HIV-negative, she’s growing up well, and this year she’ll turn 13. It’s possible to have healthy children when you follow the proper treatment.”
Germana Toni, who is receiving antiretroviral treatment at Mocímboa da Praia rural hospital, found out she was HIV-positive when she first became pregnant. Receiving support from a mãe mentora was essential for her to keep on with her treatment throughout her pregnancy.
“Cristina has always treated me with kindness and respect, offering valuable advice that motivates me to continue my treatment,” says Germana. “I encourage women and the community at large: if you test positive for HIV, it’s best to start treatment right away to ensure a healthy life.”
Building a supportive community
Working together, healthcare workers like Dr Januário and Cristina Virgílio are making strides toward breaking down stigma and creating a safe environment for people affected by HIV. Their work highlights the importance of community-driven solutions in addressing both the medical and social challenges of HIV care in conflict settings.
However, Dr Januário stresses that there is a critical need for broader support. To ensure that every HIV-positive person affected by the conflict in Cabo Delgado can access consistent, lifesaving treatment, more resources and collective action are essential.