For the past four months, the Great March of Return demonstrations in Gaza, Palestine, have been met with lethal force by the Israeli army. While the numbers of protesters and casualties have now decreased, the violence is not over – fresh gunshot wounds occur every week.
Médecins Sans Frontières (MSF) has been at the forefront of the emergency response since the start, providing both surgical and post-operative care.
The biggest challenge today is the massive cohort of patients with extremely severe injuries, which will require very advanced medical intervention and will change their lives forever.
In the operating theatre at Friendship Hospital in Gaza City, two MSF surgeons were 90 minutes into what was meant to be a 90-minute operation, struggling with what they had found. The patient’s shin had been shattered by an Israeli bullet, the bone shredded and a big chunk of flesh blown away.
The plan had been to take some healthy muscle from the calf to help fill the wound. However, once Camille Rodaix and Jan Wynands, the two MSF surgeons, opened the calf, they found that the muscle there was also damaged: riddled with bits of shrapnel and toughened by areas of scar tissue.
The problem the two surgeons were trying to treat has reached epidemic proportions in Gaza recently. Since the end of March, the “Great March of Return” protests have seen over 150 Palestinians shot dead by the Israeli army, as well as over 4,100 injured by Israeli bullets. Since the protests began, MSF has treated over 1,700 patients, nearly all of them with gunshot wounds.

The majority of these wounds were caused over just 23 days within the last four months, as most protests and Israel’s subsequent response take place on the Friday of each week. MSF is still receiving new patients as the violence has not stopped, although it is now happening on a smaller scale. Still, hundreds of Palestinian protesters are wounded every week at the fence, and a few are killed.
“The injuries that we see are characterised by a high prevalence of open fractures – most below the knee – with massive tissue loss, which means damage to the veins and nerves as well,” says Marie-Elisabeth Ingres, MSF’s head of mission in Palestine. “Many of these patients require multiple surgeries just to close the wound.”
That was the aim with the patient on the table at Friendship Hospital. “My goal is to stabilise the wound so that we can see if the bone will heal,” Camille, an orthopaedic surgeon, said as she inspected the patient’s leg, the wound on which was still raw nearly two months after the patient had been shot. An external fixator – a metal rod attached at right angles to pins drilled into the remaining parts of the bone – was keeping the shattered parts of the bone in place.

“I operated on this patient before to remove a bone fragment that was sticking up into the skin,” Camille explained, “and now I will work with Jan – a plastic surgeon – to check for any remaining bits of dead bone and to close the wound.” Though this was not the patient’s first operation, it would also not be his last: the orthopaedic surgery necessary to permanently heal the wound is “really hard,” says Camille. “We don’t have the tools to do it, and we cannot try to fix the bone while the wound is still open anyway.”
The stakes for patients like the one Camille and Jan were operating on are high. With a health system that has been crippled by more than ten years of an Israeli blockade and Palestinian political infighting, the specialist surgeries that many of these patients need are unavailable, raising the spectre that they will be disabled for life.
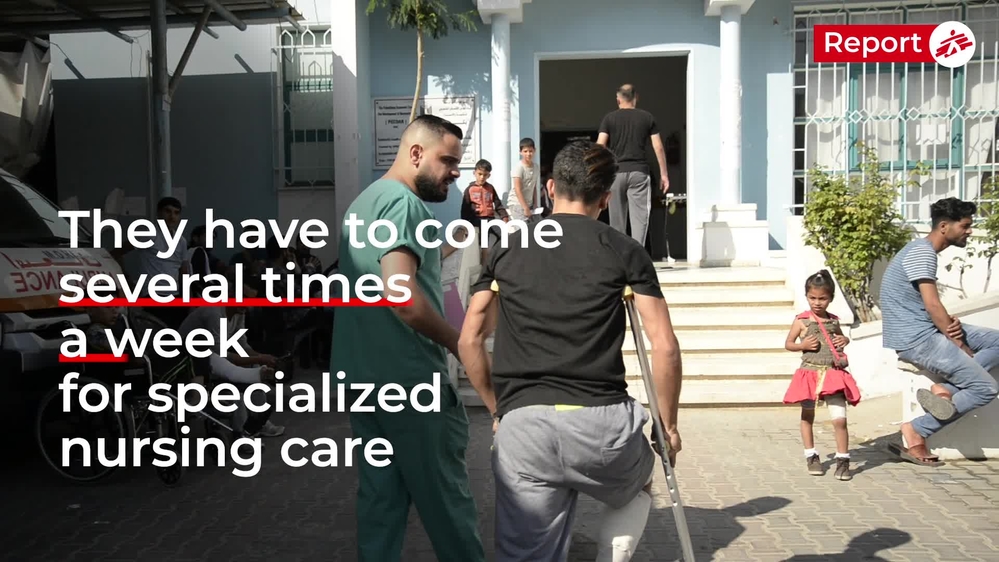
Each morning at five clinics in the Gaza Strip a succession of MSF vans pull up and discharge waves of young men, awkwardly slinging themselves out of the vehicles while holding legs forced straight by a tangle of metal. They pick their crutches from the pile that have tumbled together and propel themselves through the doors. Inside, rows of patients wait to be seen, their external fixators sticking through tracksuit bottoms lovingly stitched to have Velcro flaps that allow for the trousers to come on and off, without disturbing the pins stuck into the bone beneath.
It is in these clinics that MSF is changing dressings and providing physiotherapy, on a scale that reflects the staggering quantity and severity of the injuries. Since 30 March 2018, MSF has carried out over 40,000 appointments to change dressings for trauma patients, helping those who can to recover and keeping an eye on people whose injuries mean they require further surgery.
A day in an MSF clinic in Gaza
“I didn’t feel anything at first, when I got shot,” says Raed Bordini, 24, from al Maghazi camp. “There was just a flash of something like electricity. I sat down suddenly and found I couldn’t move. I was trying to pull myself back but I couldn’t. I was bleeding a lot, and I was scared of the effects on my leg because it was all open – cut open from the back to the front.”
Raed comes to the clinic multiple times a week for dressing changes and his external fixator is still in. “I am in a lot of pain,” he says. “I take a lot of things like ibuprofen and paracetamol, but it has no effect. I am scared the function won’t return to my leg. It scares that I’m not able to stand on it. I can see that it’s not right.”
My eyes were open but I couldn’t see. The people thought I was dead.Dawlet Hamidiyyeh, a patient shot during the protests on 14 May
Dawlet Hamidiyyeh, 33, is one of the comparatively few female patients that MSF is treating for a gunshot wound. She attends the Beit Lahia clinic in a wheelchair, her leg stuck out straight in front of her. “It was the first time I went to the fence,” she says of 14 May, the deadliest day of protests. “I wanted to see what was happening. I brought the guys some water and some perfume for the effects of the gas. After I was shot, I was taken to the Indonesian hospital. My eyes were open but I couldn’t see. But I could hear everything. The people thought I was dead. They put me in the morgue at the hospital, but after ten minutes one of the doctors noticed I was alive and started shouting that I had a pulse.”
Dawlet has to come to the clinic three times a week to have her dressings changed. Her external fixator will be in for at least five months, and she is fearful for her future: “I’m scared that I won’t be like before, that I won’t be able to walk.”

Unfortunately, the worries of many patients like Raed and Dawlet are well founded. “We will probably see a second wave of amputations,” says Pascale Marty, MSF’s medical team leader in Gaza. “Gunshot wounds are by definition contaminated wounds, because the bullet has entered the wound, meaning that there is a high prevalence of infection.” Infected open fractures of such complexity pose a threat to the life of the patient, leaving little other choice but to amputate if reconstructive surgery is not an option.
While such severe wounds and high rates of infection would generally require the patient to be admitted to hospital, the overburdened health system in Gaza cannot accommodate such a high number of patients. Mohammed Abu Gaza, 25, was shot on 6 April near Rafah. His knee shattered, but he was repeatedly discharged from hospital.
Six days after I was shot I was discharged to make space for the wounded from the next Friday.Mohammed Abu Gaza, shot on 6 April near Rafah
“I kept going back to the hospital with fever and pain but they wouldn’t admit me, because they were full.” After being referred by MSF to a different hospital, he had another operation but eventually the same thing happened: “I stayed one week there, but then they discharged me again to make way for the next wave of wounded.”
The effects of the wounds are rippling out through Gaza’s population, burdening the wider society with the costs and responsibilities of care, in a place where years of occupation, war and blockade have brought the economy to the brink of collapse. Unemployment among the 15-29 age group – which makes up two-thirds of MSF’s patients – has reached 60 per cent, according to the World Bank. Families have either lost their source of income, or for those that already had to support unemployed family members, they are now bearing the extra load of care.
“Before I was injured I sometimes sold vegetables from a cart in the market, but it was only enough to bring me money for cigarettes,” says Mohammed. “Now I just sit in the house – I can’t do anything by myself, even washing. I have to ask the family for help with everything.”

Another patient, A, who was shot on 30 March, described how his father, a government employee, had to borrow $1,500 from relatives to pay for the treatment he needed. “Before, sometimes I worked with my friends and relatives on building sites. I really miss this. I am not able to earn money now. My relatives abroad are sending money for my treatment.”
The consequences are not just economic. As well being a hairdresser, a job she had done for the past ten years, Dawlet was a caregiver for her sick father. “It hurts me that I can’t help my dad,” she says. “Now I need care as well as him.” The accumulation of physical pain, financial stress and social pressures is causing mental difficulties for many of the patients. “It’s hard 24-hours a day. I’m just sitting in the house. Honestly, it’s destroyed my life, and the life of my family,” Dawlet says, looking downcast.
While protests continue on the border every weekend and some Palestinians continue to be killed and injured by the Israeli army, the numbers are fewer. Yet the nature of the violence has evolved and escalated in recent weeks, resulting in the death of one Israeli soldier in mid-July, and continuing deaths and injuries among Palestinians.
Over two months have passed since the days of the heaviest casualties, a period of time that would see normal fractures heal. For many of those in Gaza, progress has not nearly been so quick, due to the complexity of their injuries.

“They will need five to six months to heal, if they heal at all,” says Camille, the orthopaedic surgeon. “Our patients can be divided into three groups of roughly equal sizes: those who will eventually heal, those who will need extra surgeries to heal, and those who will need specialist reconstructive surgery over the course of years if they are to have any chance of healing.”
This type of surgery is unavailable in Gaza, leaving many people facing the possibility that they will never regain the function of their limbs.
Back at Friendship Hospital, after some tense moments Camille and Jan succeeded in pulling across the section of muscle they needed to fill their patient’s wound. A section of the skin from the thigh had been grafted onto the wound to close it, and the team started to relax as the long hours of surgery came to an end.
“This operation was typical,” said Camille. “You think, ‘This is not so bad,’ but the wounds are so bad here that you never know what you will find inside.” She is hopeful that the patient will manage to avoid further infection with the wound closed. However, for him and many others, with bones missing and the blockade in place, the long-term future is far from certain.






