Dense, cramped living conditions, poor quality water and inadequate vaccination coverage have left Rohingya refugees prone to outbreaks of contagious diseases. MSF’s preparations for upcoming cyclone and monsoon season are ongoing.
Rohingya still vulnerable to serious health risks
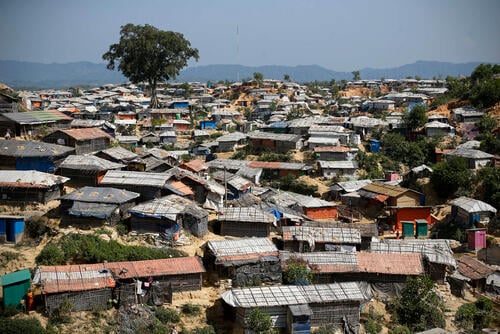
In August 2017, more than 700,000 Rohingya began crossing the border into Bangladesh, fleeing violence in Myanmar. Twenty months have passed and the refugee population, living in camps across Cox’s Bazar, remains vulnerable to serious health risks. Rohingya refugees reside in overcrowded, tight spaces and continue to live in emergency-like conditions, which increase the threat of potential outbreaks of contagious diseases.
Vaccination coverage
The prevalence of vaccine-preventable diseases among the population highlights their poor levels of vaccination, while a high number of incidences of acute watery diarrhoea indicate the poor quality of water and limited access to sanitation facilities. Between August 2017 and March 2019, MSF treated 7,032 patients for diphtheria, 4,987 for suspected measles and 99,681 for acute watery diarrhoea.
Vaccination coverage is generally low among the Rohingya as a result of limited access to healthcare for many years in Myanmar. To counter this, MSF has supported a number of vaccination campaigns run by the Government of Bangladesh to prevent the spread of diphtheria, measles and cholera. MSF is also working with the government to strengthen the routine expanded programme of immunisation, which is available for Rohingya children aged two years and under. The programme should be increased to include all children under the age of five.
Living conditions
MSF have undertaken a range of activities to improve public health in the refugee settlements and reduce the risk of outbreaks of disease. Since 2017, our teams have provided more than 193 million litres of chlorinated water to 77,430 people and completed the construction of five water networks and a faecal sludge management system. This included building 390 latrine blocks, desludging 760 existing latrines, treating 1,433 million litres of faecal sludge, and running almost 12,000 hygiene promotion sessions. Providing adequate water and sanitation facilities is key to protecting the health and dignity of the Rohingya.
Specialised healthcare
The lack of specialised healthcare for both refugee and host communities in Cox’s Bazar remains a serious concern. There is inadequate provision of secondary healthcare, including good-quality 24-hour surgical capacity, comprehensive obstetric and neonatal care, paediatric services, and treatment for non-communicable diseases, including mental health and chronic illnesses. MSF remains one of the main organisations providing inpatient services for paediatric, neonatal and adult patients.

Cyclone season
The cyclone and the monsoon season is due to begin in May or June. MSF’s preparations for this are ongoing. Cyclones and heavy rains can wreak havoc on the semi-permanent structures, mostly made of bamboo and plastic sheeting, that make up the majority of buildings in the refugee settlements.
Emergency measures, such as cyclone shelters, do not exist for refugees and are inadequate for the host community. MSF is putting in place a mass casualty management plan in two field-level hospitals, which will include activating our outbreak response centre and distributing non-food item kits.
Future prospects
The Rohingya are almost entirely reliant on health services provided by humanitarian organisations in the refugee camps. Increasing the ability of local healthcare providers to meet their needs will be crucial to managing the long-term health needs of the refugees and the host community.
The Rohingya have limited access to round-the-clock lifesaving surgical care within and outside the camps, and this may be further reduced over time. Patients in need of surgical procedures, for example emergency obstetrics, can be at risk when there are no nearby facilities able to admit them. Patients requiring surgery are frequently referred to facilities to either in Cox’s Bazar town, where human resources are limited, or the city of Chittagong, a journey that takes several hours by road. These delays result in many stable cases deteriorating into critical life-threatening cases.
Coping with trauma
MSF is one of the few organisations in the region to provide comprehensive mental health and psychiatric care. Many Rohingya lived through traumatic experiences while fleeing the violence in Myanmar. This, together with the lack of jobs and an uncertain future, can impact their mental wellbeing.
MSF also provides support and treatment to victims of sexual and gender-based violence at its health facilities. Since August 2017, MSF has treated more than 1,000 victims of sexual and gender-based violence. Our services include psychosocial care, treatment for people who may have been exposed to HIV and sexually-transmitted diseases, emergency contraceptives, hepatitis B vaccinations, and treatment for menstrual regulation (the Bangladeshi medical term for the care of unplanned pregnancies).
The refugee crisis has impacted public health services in Cox’s Bazar. In collaboration with the Government of Bangladesh and the Ministry of Family Welfare and Health, we are providing mental health and psychiatric care at the Ukhiya Upazila Health complex. MSF is also improving infection prevention and control, hygiene protocols and waste management inside Sadar Hospital in Cox’s Bazar.
A lack of legal status, restrictions on freedom of movement and the uncertainty about their future remain major concerns for the Rohingya and continue to affect their health. There is a greater need for coordination, and improved quality and capacity in the humanitarian response, so that long-term needs do not build up and place further strain on the local healthcare system. Adequate funding for healthcare has to be secured to address the huge gaps in access to secondary healthcare.
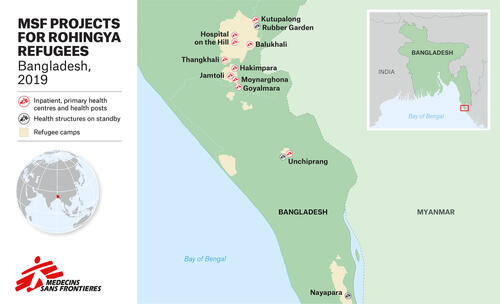
MSF activities in Cox's Bazar
Health facilities
Three field hospitals with inpatient facilities, four 24-hour primary health centres, one specialised clinic for reproductive and mental healthcare, a dedicated isolation centre for outbreak response and two fixed health posts.
Number of patients (August 2017 – March 2019)
1,242,500 outpatient consultations and 21,549 inpatient admissions, including treatment for 7,032 people for diphtheria, 4,987 people for suspected measles, 47,556 antenatal consultations, 2,750 deliveries, 1,087 victims of sexual and gender-based violence, and 25,679 individual and 41,480 group mental health consultations.
Main health concerns
Respiratory tract infections, and diarrhoeal and skin diseases.
Water and sanitation activities
193 million litres of chlorinated water available for 77,430 people, five water distribution networks, and a faecal sludge management system treating 1,433 million litres of faecal sludge, construction of 390 latrine blocks, desludging of 760 latrines, and conducting over 11,990 hygiene promotion sessions.
Outreach activities
Focus on health promotion, investigating possible outbreaks, supporting vaccination campaigns, and maintaining relations with the community and other organisations. Surveillance teams gather demographic, nutritional, mortality and birth indicators in most settlements to monitor and anticipate health needs.
Number of staff
Over 1,600 staff
Other projects in Bangladesh
MSF operates two specialised health clinics in Alinogor and Madbor Bazar in the Kamrangirchar area of Dhaka, where we run an occupational health programme for 7,000 workers in small-scale factories. Services include treating health issues related to occupational health (includes injuries), preventive tetanus vaccinations and conducting hazard prevention activities to improve workplace safety in the factories. We also provide sexual and reproductive health services, primarily focused on women under the age of 20. These services include antenatal and postnatal consultations, gynaecology consultations, nutritional support, routine vaccinations, family planning and assistance with deliveries, including caesarean births.
Victims of sexual and gender-based violence are supported with comprehensive medical care, psychosocial support and referral to external actors for legal support. MSF teams in Kamrangirchar also provide mental health support, and conduct health promotion and community engagement activities.