Health campaigners are calling for more effective, but more expensive, anti-malarial drugs to be made available across Africa. Medecins Sans Frontieres (MSF) said the failure to fund the combination drug treatment showed an emphasis on saving money rather than saving lives. Their call comes as a report by the World Health Organization (WHO) and the United Nations Children's Fund, published to coincide with Africa Malaria Day, says some 3,000 African children die every day of the disease. The WHO is also calling for wider availability of the more effective drugs - and of insecticide-treated nets, which it said can reduce malaria transmission by up to 60%.
Malaria in Africa
- Up to 3,000 children die each day
- 1-2 million people die each year
- Number of cases has quadrupled in 20 years
MSF says there has been a dramatic surge in malaria cases over the last decade. There were around four times the number of cases in the 1990s than the 1970s and two to three times the number of deaths in hospital. In large part, this is due to high levels of resistance to the drugs chloroquin and sulphadoxine-pyrithemaine (SP). Malaria kills between one and two million people across Africa each year. Overall, around $12bn is lost each year across the continent.
Highly potent
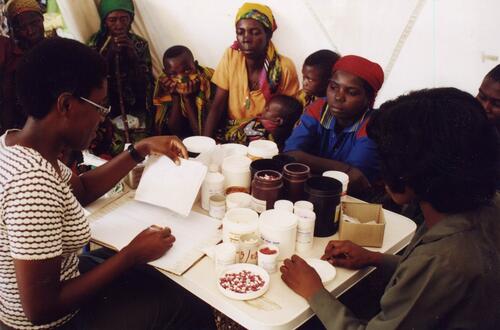
Death rates from malaria were falling until the early 1980s when resistance to chloroquin began to develop. By 1999, Tanzania had resistance rates ranging from 28 to 97%, in Kenya from 66 to 87% and from 10 to 80% in Uganda. MSF is calling on donor agencies, such as the UK Department for International Development and the US Agency for International Development to plough more money into malarial treatment in Africa. It wants them to fund the introduction of ACT - artemisinin-based combination therapy, which has been recommended by the WHO. What would you rather do - waste money on old cheap drugs that you know don't work or fund a more expensive treatment that will save lives? Dr Nick White, tropical medicines expert Artemisinin drugs, derived from the Chinese plant Artemisia annua , have been used for more than 10 years in Asia and are highly potent, fast-acting and well tolerated. In combination with other drugs such as amodiaquine, they can eradicate malaria symptoms in three days. ACT is being introduced in some African countries, including the KwaZulu Natal province in South Africa, Burundi, Zambia and Zanzibar in Tanzania. KwaZulu Natal saw an 80% reduction in hospital deaths from malaria when ACT was introduced. Other countries want to follow WHO guidance and introduce the therapy, but cannot afford it. ACT costs around $1.50 a dose, compared to 50 cents a dose for chloroquin. MSF says this could fall to around 50 to 80 cents once ACT begins to limit the spread of malaria. But it would still cost up to $100 to 200m to change to ACT treatment across Africa.
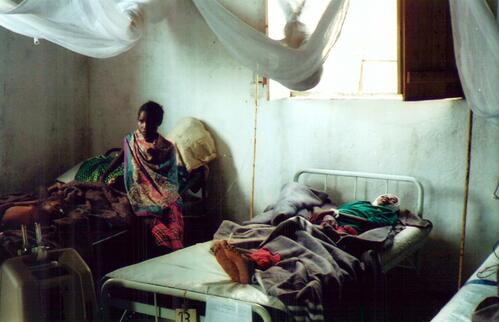
Pregnant women
Dr Christa Hook of MSF said: "The responsibility is the donors'. They must make the message very clear that they will support requests for ACT." Dr Nick White, professor of tropical medicine at Mahidol University, Thailand and Oxford University said: "What would you rather do - waste money on old cheap drugs that you know don't work or fund a more expensive treatment that will save lives?" Dr Bernard Pecoul, director of MSF's Campaign for Access to Essential Medicines, added: "Since 2001, WHO experts have recommended replacing failing malaria medicines with more effective treatments, but donors have failed to encourage this change, choosing to save money rather than lives." Carol Bellamy, executive director of Unicef, said: "Malaria kills an African child every 30 seconds, and remains one of the most important threats to the health of pregnant women and their newborns. "We have the knowledge and the potential to achieve our target of reducing the global burden of malaria by half by 2010, but we need much greater investment and political commitment."
A conference is to be held in London on Friday to mark Africa Malaria Day, where the Roll Back Malaria Partnership will publish its first comprehensive report on malaria across the continent.