We treat patients suffering from a wide array of illnesses and health needs. Here you will find some of the main needs we see and what we do about them.
Discover the main crises we work in, the consequences faced by affected people and challenges in delivering care.

Access to medicines
Unaffordable, unavailable, not adapted - people around the world face these challenges in accessing lifesaving medicines.

Antibiotic resistance
Antibiotic resistance is a serious and growing phenomenon in contemporary medicine and has emerged as one of the pre-eminent public health concerns of the 21st century.

Attacks on medical care
Attacks against medical facilities and health workers, whether deliberate or indiscriminate, are part of generalised violence and atrocities committed against civilians in armed conflict. They deprive populations of health services, often when they need them the most.

Central American migration
An estimated 500,000 people a year flee violence and poverty in El Salvador, Guatemala, and Honduras, heading north through Mexico to find safety. The levels of violence in the region are comparable to that of war zones MSF has worked in for decades.

Child health
Around the world, Médecins Sans Frontières (MSF) teams are working to protect the health of children.

Cholera
Although easy to prevent and treat, cholera affects up to 4 million people worldwide per year, resulting in up to 140,000 deaths.

Climate emergency
The health impacts of a changing climate are already a burden for many people in the world, including those MSF teams assist.

Conflict in Sudan
Find out the latest information on MSF's response to the conflict in Sudan.

Coronavirus
Coronaviruses are a large family of viruses, most of which are harmless for humans. However, two types can cause severe lung infections. MSF is currently responding to a worldwide coronavirus pandemic, COVID-19

Epidemics and pandemics
Millions of people still die each year from infectious diseases that are preventable or can be treated.

Gaza-Israel war
Learn how MSF teams are responding to the Hamas-Israel war in Gaza, Palestine.

Haemorrhagic fevers
Ebola and Marburg haemorrhagic fevers are rare but deadly. Outbreaks can kill 25 to 90 per cent of those infected, spreading fear and panic among affected communities.
Hepatitis C
Worldwide, an estimated 58 million people are infected with the hepatitis C virus, with about 1.5 million new infections occurring per year. While hepatitis C can be cured, few people have access to treatment.

Hepatitis E
Hepatitis E is transmitted by ingesting water contaminated by an infected person’s faeces. Outbreaks are often documented in places with poor sanitation, like camps for refugees and internally displaced people (IDPs). Hepatitis E commonly causes only a mild short-term illness.

HIV/AIDS
Around 630,000 people died from HIV-related causes, while 1.3 million people became newly infected with the HIV virus in 2022.

Kala azar
Hundreds of millions of people are at risk of infection with kala azar - one of the world's most dangerous parasitic diseases. Only malaria is more deadly.

Malaria
Each year, malaria kills over 600,000 people. Three-quarters of all deaths are children under five years of age.

Malnutrition
More than 224 million children around the world last year suffered from malnutrition. It is the underlying contributing factor in nearly half of the deaths of children under five years of age.

Measles
In 2023, our teams vaccinated 3.3 million people against measles in response to outbreaks. But the highly contagious viral disease remains one of the leading killers of young children.

Mediterranean migration
Every year, thousands of people fleeing war, persecution and poverty at home attempt the treacherous journey across the Mediterranean. Countless lives are lost on the way.

Meningitis
Meningococcal meningitis is a highly contagious bacterial form of meningitis – a serious inflammation of the meninges – the thin lining that surrounds the brain and spinal cord.
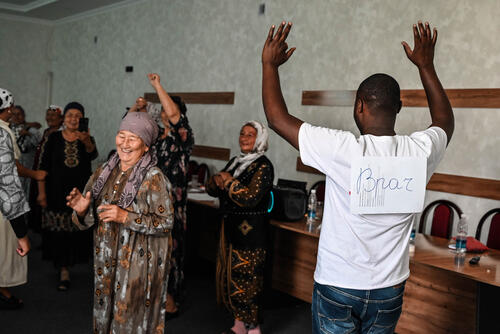
Mental health
Where we work, we may see people with a mental illness or confronting distressing situations, such as violence, loss or displacement. Mental health support can be crucial to help people cope.

Mpox
Learn more about MSF's activities in responding to mpox.

Natural hazards
Within a matter of minutes, natural hazards can affect the lives of tens of thousands of people. Hundreds or even thousands of people can be injured, homes and livelihoods destroyed. Access to clean water, healthcare services and transport can also be disrupted. The impact of each event varies greatly and our response must adapt to each situation.

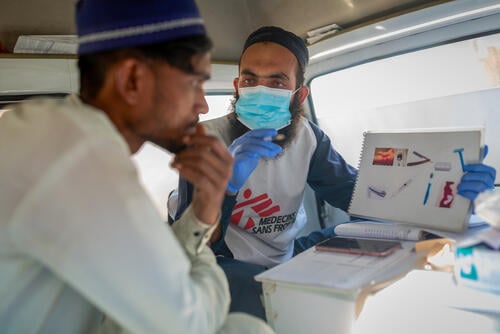
Independent medical humanitarian assistance
We provide medical assistance to people affected by conflict, epidemics, disasters, or exclusion from healthcare. Our teams are made up of tens of thousands of health professionals, logistic and administrative staff - most of them hired locally. Our actions are guided by medical ethics and the principles of independence and impartiality. We are a non-profit, self-governed, member-based organisation.
Learn more

