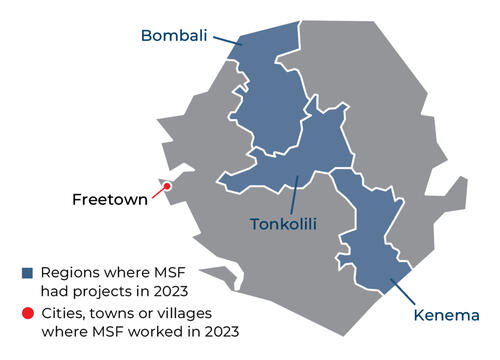
In Sierra Leone, we work in Kenema district to reduce high maternal and child mortality rates, providing pre- and post-natal care in our hospital. We also provide care to remote villages in the district through mobile clinics.
Our activities in 2023 in Sierra Leone
Data and information from the International Activity Report 2023.
1,426
1,426
€17.6 M
17.6M
1986
1986

152,000
152,
27,100
27,1
11,800
11,8

2,150
2,15

New approach improves diagnosis and treatment of children with TB in Sierra Leone
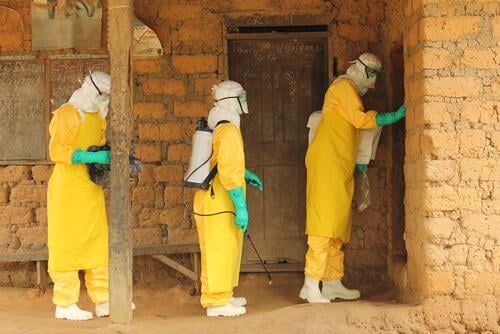
Five things to remember a decade after the Ebola outbreak in West Africa

Helping pregnant women access timely and quality maternity services

New hospital to counter high maternal and child mortality rates

Lassa fever: A challenging disease to diagnose and treat




