Since MSF first responded in Sierra Leone – during a cholera outbreak in 1986 – we have adapted and expanded our projects to meet the growing needs in the country. Today, our teams monitor the spread of different diseases, including COVID-19, and is helping to boost the pool of skilled and qualified medical staff.
In a country where child and maternal death rates are exceptionally high, our activities are focused on children under five, pregnant women and lactating mothers, especially in Kenema, in the country’s east.
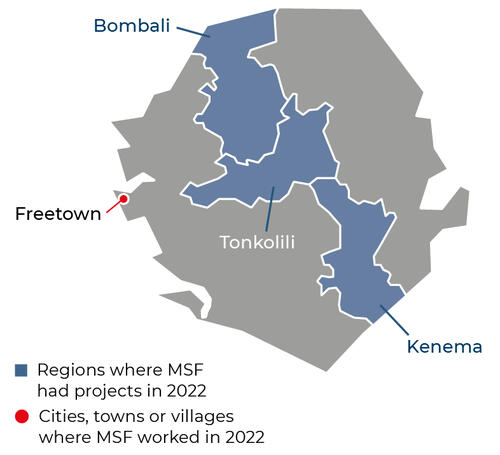
MSF currently runs medical projects in three districts, Kenema, Tonkolili and Bombali, helping the Ministry of Health and Sanitation to provide general and specialist healthcare, including for tuberculosis and HIV. Our teams also provide psychosocial support and treatment for victims of sexual and gender-based violence.
To address the lack of skilled and qualified health workers, the MSF Academy has enrolled nurses and clinical heath officers in Kenema, to help improve the services and to deliver effective responses during emergencies.
What are we doing in Sierra Leone?


Across all age groups, malaria is the country’s single biggest killer, accounting for 38 per cent of hospital admissions. Children are particularly vulnerable to malaria. In Sierra Leone, MSF treats malaria at Hangha hospital in Kenema district, and through mobile clinics that reach 25 villages in Kenema.


Outbreaks and civil war have severely weakened Sierra Leone’s health system. Children are affected by malaria, malnutrition, diarrhoea and skin diseases. To help address the burden of preventable disease and monitor disease outbreaks, MSF is part of the case management and surveillance group at the Sierra Leone Emergency Operations Centre.


Our activities focus on providing healthcare for children under the age of five in Hangha hospital, including therapeutic feeding for malnourished children, and general paediatric care. Our teams also provide care for pregnant and lactating women, including the prevention of mother-to-child HIV transmission. A new maternity ward in Hangha hospital includes two operating theatres for complicated deliveries and a neonatal unit.


MSF outreach teams are delivering community-based medical care directly to people in 25 remote and hard to reach villages to address medical issues such as malaria, diarrhoea and pneumonia in Kenema district, through 10 local health units set up in these areas. Our activities also include ensuring consistent supplies of essential drugs, medical consultations, child vaccinations and health facility rehabilitations.
Our activities in 2022 in Sierra Leone
Data and information from the International Activity Report 2022.
1,448
1,448
€20.1 M
20.1M
1986
1986

137,600
137,6
86,200
86,2
5,190
5,19

74
74
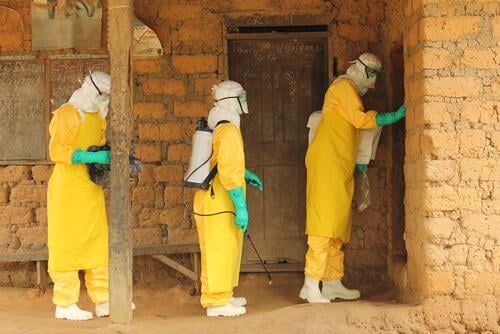
Five things to remember a decade after the Ebola outbreak in West Africa

Helping pregnant women access timely and quality maternity services

New hospital to counter high maternal and child mortality rates

Lassa fever: A challenging disease to diagnose and treat

Learning from the past, preparing for the future





